Sunday, November 27 | 11:25 a.m.-11:35 a.m. | SSA16-05 | Room N226
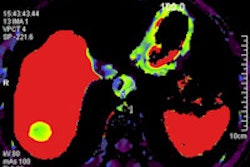
CT perfusion imaging of the brain is often used in acute stroke centers to aid in diagnosing and characterizing acute stroke. But it doesn't work as well in the brainstem: A new study has found that CT perfusion alone is inadequate to detect basilar artery occlusion.The use of CT perfusion is well-established despite difficulties in standardizing the technique, explained Dr. Jeffrey Carpenter to AuntMinnie.com.
"In the anterior circulation, threshold values indicative of viable versus nonviable brain have been proposed, although in reality most stroke specialists interpret the results qualitatively," he said. "This qualitative assessment usually involves comparing values in the affected region with the contralateral brain."
However, the opportunity to double-check the interpretation via the contralateral side is usually missing in the brainstem, he said. In addition, brainstem imaging includes surrounding dense bone, which increases noise.
But patients with basilar artery occlusion can present with symptoms very similar to anterior circulation strokes, so they get imaged like all the other stroke patients; that is, noncontrast CT, plus CT angiography, plus CT perfusion.
Carpenter and colleagues from West Virginia University aimed to answer the question of how well CT perfusion characterizes basilar artery occlusion. The answer is that it does not do it very well, Carpenter reports. Six of the 19 basilar artery occlusions were not detected by CT perfusion using all levels.
"Despite choosing the least subtle brainstem stroke to study, CT perfusion in its current form can not only fail to characterize a stroke as we do in the remainder of the brain, [it] utterly fails to detect it," he said. That means that CT and CT perfusion are not adequate in the setting of basilar artery occlusion and should always be performed with CT angiography, which can "at least depict the obstruction, and if the patient is not obtunded [he or she can] be taken to the angio suite for recanalization," he said.
If posterior stroke is suspected and MRI is available, the MRI would be preferable, he said.