CT versus MRI -- the latter is the obvious choice for children because MRI does not use ionizing radiation, right? Actually, CT can be safer depending on the exam, say researchers eyeing the comparative risks of the modalities.
Changes in practice and CT technology over the past decade require a re-examination of risk perceptions about MRI and CT angiography in children, according to Dr. S. Bruce Greenberg, professor of radiology and pediatric medicine at the University of Arkansas for Medical Sciences.
In a talk at the 2011 International Society for Computed Tomography (ISCT) annual meeting, Greenberg said that CT doses have dropped dramatically in recent years, while the risks associated with some MRI scans, which more commonly require general anesthesia or deep sedation, have been underplayed.
In addition to cardiac MRI studies, interoperative MRI procedures under anesthesia are gaining traction for a variety of surgical and interventional tasks.
"MRI under general anesthesia is not safer than low-dose CT angiography," Greenberg said.
CT risks fall with dose
The first perception that needs to be re-examined involves just how relevant it is to take cancer risks calculated in nuclear bomb survivors and apply them to the exposure of children undergoing CT to ionizing radiation, Greenberg said.
Nuclear bomb survivors have a known increased cancer risk that is proportional to the degree of radiation exposure they received over a range of radiation doses. But these doses are beyond the exposure of most diagnostic imaging scans, he said. Still, there is some overlap with CT if adult CT techniques are applied to children.
The risks associated with CT are based on several assumptions: principally, that the average effective dose of a diagnostic scan is assumed to be 10 mSv, with an increased risk of cancer death calculated at 5% per sievert of radiation.
"The assumptions mean that approximately one additional cancer death will occur for every 2,000 scans," he said, a level that would eventually account for 1.5% to 2% of future cancer deaths in the U.S. Although 7% of CT scans are performed on children, their greater sensitivity and longer life expectancy could result in up to 15% of future cancer deaths.
But it's time to correct this perception in light of the past decade's reduction in radiation exposure, Greenberg said.
"Increased use of pediatric protocols that reduced kVp and mA have dramatically reduced radiation exposure to children," he said. In addition, newer technologies such as wide-detector scanning, denoising filters, and iterative reconstruction should lead to further reductions in radiation exposure during CT.
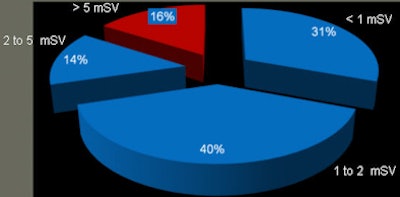
Take cardiac CT, one of the higher-dose techniques available for evaluating cardiovascular disease in children. Data showing the effective CT angiography doses during the past year at Arkansas Children's Hospital indicate that more than 70% of the studies used less than 2 mSv. Eighty-four percent of the studies were less than 5 mSv, Greenberg said.
 |
| Pie chart shows the calculated effective doses during the past year at Arkansas Children's Hospital. All studies used a wide-detector scan technique, but they did not use other potentially dose-saving techniques such as iterative reconstruction or denoising filters. More than 70% of the studies used less than 2 mSv, while 84% used less than 5 mSv. Image courtesy of Dr. S. Bruce Greenberg. |
That level -- 5 mSv or less -- is important with respect to the nuclear bomb survivor data, Greenberg said, because the risk calculations have changed.
Updating risk
Assigning dose exposure to the nuclear bomb survivors is based on dose shielding (DS) models, Greenberg explained. Projections of elevated cancer risk in patients undergoing CT used nuclear bomb survivor data based on the old DS 86 model, which underestimated gamma radiation exposure by about 10%.
The model was superseded by the DS 02 model, and in a 2004 paper (Radiation Research, October 2004, Vol. 162:4. pp. 377-389), Preston and colleagues recalculated the risk of additional cancers. One of the subgroups included survivors who received less than 5 mSv of radiation. This group was compared to a group that received no radiation.
The group with CT radiation doses of 5 mSv or less actually had 12 fewer solid cancers than the control group, but the CT group also had seven more leukemia cases than the control group, Greenberg said.
"Clearly, the data indicate that no measurable increased cancer rate exists for nuclear bomb survivors who received less than 5 mSv of exposure," he said. "The existing data do not support a linear no-threshold model."
This conclusion, which enjoys broad support in the larger scientific community, doesn't exclude some increased risk due to low-dose radiation, but it "makes the linear no-threshold model an act of faith rather than science," he said.
Other perceptions that need revising are those surrounding the safety of MRI, Greenberg said. Because MRI does not use ionizing radiation, it is seen by some as the panacea for the problems of CT, and while the modality's anesthesia risk is acknowledged, it is perceived to be small. Interoperative MRI is becoming more common for a variety of surgical procedures.
But the anesthesia risk for children undergoing MRI can be categorized as acute and long term.
Recent literature in anesthesiology shows that "children are more vulnerable to respiratory depression, and they have more atelectasis than adults undergoing general anesthesia," Greenberg said. "Neonates are particularly at risk, having increased fluctuations of heart rate, blood pressure, and oxygen saturation" (Serafini et al, Current Opinion in Anesthesiology, August 2008, Vol. 21:4, pp. 499-503).
Certainly the overall risk of patients undergoing MRI is low: The death rate is only 5.3 deaths per million studies, Greenberg said. But in a study looking at children undergoing MRI with general anesthesia, which is often needed due to longer scan times, the death rate was found to be one per 3,900 exams (Anesthesiology, March 2009, Vol. 110:3, pp. 459-79).
"This was found to be twice as dangerous as doing general anesthesia in the operating room," he said.
In the long term, general anesthesia has an effect on the developing brain, causing both γ-aminobutyric acid receptor agonism and N-methyl-D-aspartate receptor antagonism.
"These changes result in mitochondrial membrane permeability disruption leading to neuroapoptosis," he said. The youngest children are most at risk, as sensitivity peaks during the period of synaptogenesis, which begins during the last trimester of pregnancy and continues during the first two years of life, he said.
Indeed, an article published in the August edition of Current Opinion in Anesthesiology notes that general anesthesia depresses neuronal activity and communication during synaptogenesis, leading to long-term cognitive impairment, wrote Dr. Vesna Jevtovic-Todorovic, PhD, professor of anesthesiology at the University of Virginia Health System.
"Although clinical importance remains to be substantiated, results to date do indicate that exposure of animals to general anesthesia during active synaptogenesis is most detrimental," she wrote (Curr Opin Anaesthesiol, August 2011, Vol. 24:4, pp. 395-399).
More studies on the long-term effects of anesthesia and sedation will be coming out in the next couple of years, "so we're going to have to evaluate risks again," Greenberg said. So what's the right choice today?
"What we can say is that a low-dose CT exam -- anything less than 5 mSv -- does not have any measurable increase in cancer risk," he said. "MRI under general anesthesia is not safer than low-dose CT angiography. Our challenge in the future is to develop MRI protocols that are less dependent on anesthesia, and for CT to continue to ratchet down radiation to lower and lower doses."