A study published January 6 in the American Journal of Respiratory and Critical Care Medicine confirms earlier reports suggesting that statin use in current and former smokers is associated with interstitial lung abnormalities (ILA) detected on CT scans.
In new findings from the COPDGene trial of current and former smokers, 38% of subjects who were taking statins had lung abnormalities detected on CT, compared with 27% of subjects who weren't taking statins. (The COPDGene study is funded by the U.S. National Institutes of Health and uses CT and other diagnostic tests to explore the mechanisms behind chronic obstructive pulmonary disease [COPD].)
"Our findings in a large cohort of smokers demonstrate that statin use may increase the risk of developing radiographic evidence of [interstitial lung disease] including findings characteristic of pulmonary fibrosis," wrote Dr. Jin-Fu Xu and colleagues from Brigham and Women's Hospital in Boston (AJRCCM, January 6, 2012).
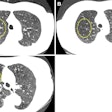
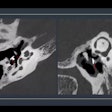
CT patterns of lung disease
Interstitial lung disease (ILD) refers to a group of respiratory diseases characterized by varying degrees of pulmonary interstitial fibrosis and inflammation at CT. Earlier findings in the COPDGene study showed that current and former smokers demonstrated chest CT patterns of increased lung density, even though they were not previously diagnosed with lung disease (Academic Radiology, January 2010, Vol. 17:1, pp. 48-53). That study found that individuals with these CT abnormalities also had reductions in total lung capacity and higher rates of respiratory symptoms, necessitating further exploration.
Statins are commonly prescribed for treating hypercholesterolemia and for the long-term prevention of morbidity and mortality from coronary artery disease. But the drugs' role in the development of interstitial lung disease remains controversial.
"While some studies evaluating both human lung fibroblasts and mice suggest that statins could be beneficial in the treatment of fibrotic lung disease, contrasting observations suggest that statins enhance monocyte secretion of inflammasome-regulated cytokines ... that may play important roles in the progression of pulmonary fibrosis," Xu and colleagues wrote.
The group used regression analyses to evaluate the association between statin use and interstitial lung abnormalities in a large cohort of smokers from COPDGene, hypothesizing that statins would increase the risk for ILA in populations of smokers. The study also included a separate arm in which the researchers analyzed the impact of statin pretreatment in a mouse model to explore the biological mechanism that might be causing the phenomenon.
For the human arm of the study, the researchers used multivariate analyses to study the relation between lung abnormalities detected on CT and statin use, all modeled for age, sex, pack-years of smoking, presence of COPD, presence of high cholesterol or heart disease, and other variables. Statin use was positively associated with interstitial lung abnormalities at an odds ratio of 1.60 (95% confidence interval: 1.03-2.50, p = 0.04) after being adjusted for covariates including a history of high cholesterol or coronary artery disease.
In the second arm of the study, the mouse model showed that statin administration aggravated lung injury and fibrosis in mice treated with bleomycin. The mouse experiments also showed that statins enhanced NLRP3-inflammasome activation by increasing mitochondrial reactive oxygen species (MtROS) generation in macrophages, resulting in increased inflammasome-mediated immune response, which could lead to fibrosis.
The new study differs from previous research and case reports that were limited by small sample size, the potential for selection bias in controls, or case selection based on diagnostic code alone. The data also support an association between cardiovascular disease and the development of fibrotic lung disease, but "several lines of evidence" suggest that cardiovascular disease alone is not likely to be entirely responsible for the findings.
The authors cautioned clinicians against using their findings to change management of patients, such as by withdrawing the use of statins. Instead, clinicians should keep in mind that signs of lung abnormalities can appear on imaging studies of these types of patients.
"While increases in the risk of ILA, and radiologic features of pulmonary fibrosis, are causes for concern, these risks do not likely outweigh the substantial benefits of statin therapy in patients with cardiovascular disease," the authors wrote. "In addition, our findings do not rule out the possibility that statin use could benefit some patients with respiratory disease. Instead, we believe that clinicians should be aware that radiographic evidence of interstitial lung disease, much like myopathy, can occur in some patients on statins."