Dual-source CT (DSCT) can compete with MRI and SPECT in the performance of sophisticated cardiac scans that combine anatomic and functional imaging for a comprehensive assessment of patients with suspected coronary artery disease, say researchers from Spain and the U.S.
CT not only differentiates between healthy and diseased myocardium, it allows evaluation of both qualitative and semiquantitative parameters, they said. In a head-to-head matchup with MRI and SPECT in patients with suspected cardiac disease, DSCT showed high sensitivity, specificity, and positive and negative predictive values for detecting even minor myocardial perfusion defects, which where mapped and color-coded to correspond to SPECT studies, said Dr. Markus Weininger, from the Medical University of South Carolina in Charleston, in a presentation at the 2011 RSNA meeting.
Half the job
CT has demonstrated high accuracy in detecting coronary artery stenosis, Weininger said. But anatomic assessment performed by most centers is only half of the job the modality will need to perform to manage patients with suspected coronary artery disease.
"In its current form, cardiac CT's diagnostic value for evaluation of the functional significance of detected stenosis is limited because of its restricted ability for a complete dynamic evaluation of contrast medium passage through the myocardium, and because a strict morphological evaluation of the anatomy is inadequate for a comprehensive assessment of all aspects of coronary artery disease," Weininger said.
Advances in CT technology now make it feasible for imaging correlation of all aspects of coronary disease, "including a detailed morphological assessment of the coronary arteries and hemodynamic evaluation of detected stenoses," he said.
To that end, investigators from the Medical University of South Carolina and the University of Navarra in Pamplona evaluated the feasibility of stress myocardial perfusion imaging using second-generation DSCT for qualitative and quantitative assessment of myocardial blood flow, compared to MRI and SPECT.
 |
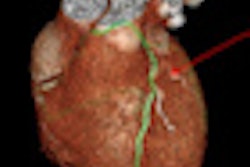
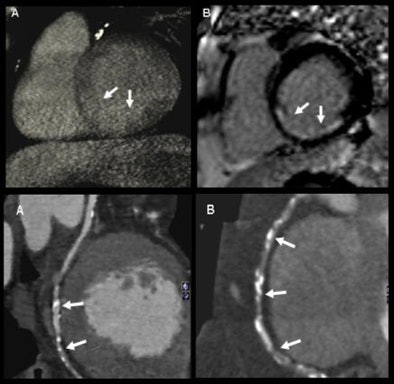
| In a 51-year-old man with suspected coronary artery disease, rest and perfusion CT (above) shows a hypoperfused blue color-coded area inferoseptally, in results that are well-correlated to both SPECT and MRI. In the same patient the results showed delayed contrast enhancement at both CT and MRI, coronary CT angiography revealed calcified plaques in the corresponding coronary artery. |
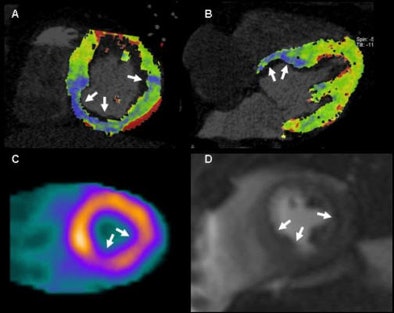 |
 |
The researchers examined 30 patients (18 men, 12 women; ages 51-76; mean age, 62 ± 12) using a standardized-protocol triphasic cardiac CT scan that included prospectively electrocardiogram-triggered coronary angiography, dynamic stress myocardial perfusion imaging, and delayed-enhancement imaging. Each patient also underwent stress and rest perfusion MRI, and delayed-enhancement MRI and SPECT, he said.
Scanning with DSCT (Somatom Definition Flash, Siemens Healthcare), the researchers started their imaging sequence three minutes into adenosine stress (regadenoson, 140 µg/kg/min) using a dynamic scanning mode with image acquisition at two automatic table positions and the table shuttling back and forth between the two positions, Weininger explained. Images were acquired at 100 kV and 300 mAs, with a 10% overlap between both acquisition ranges, resulting in 73 mm of anatomic coverage.
The imaging sequence was started four seconds prior to the bolus (50 mL contrast, 50 mL saline chaser at 6 mL/sec flow rate) to ensure a baseline acquisition of noncontrast-enhanced images -- similar to what's done with MRI, Weininger said.
The results were compared in three types of analysis:
- Qualitatively: visual interpretation of CT perfusion in conjunction with delayed-enhancement CT, MRI, and SPECT
- Semiquantitatively: analysis of short-axis reformats using software (Argus, Siemens), compared to perfusion MRI
- Quantitatively: calculation of myocardial blood flow using prototype software (syngo Volume Perfusion, Siemens)
In the quantitative analysis, CT perfusion correctly classified 54 perfusion defects of the 60 identified by MRI, yielding 86% sensitivity and 98% specificity. At the semiquantitative analysis, the group found significant differences in the upslopes of the signal intensity of the time curve between normal and ischemic myocardium of both CT and MRI, Weininger said. In the absolute quantification of myocardial blood flow, CT was again able to differentiate between normal and ischemic myocardium, he said.
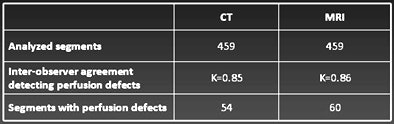 |
| Qualitative analysis: CT perfusion correctly classified 54 perfusion defects. Values for detecting myocardial perfusion defects at CT (versus SPECT) compared to MRI were as follows: 86% (84%) sensitivity, 98% (92%) specificity, 93% (88%) positive predictive value, and 94% (92%) negative predictive value. |
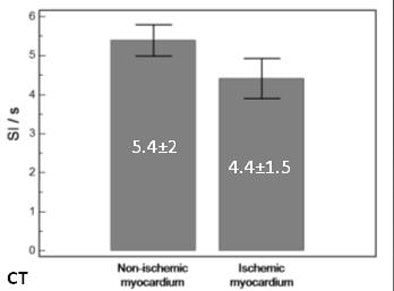 |
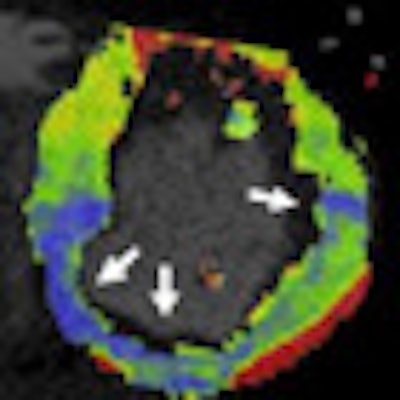
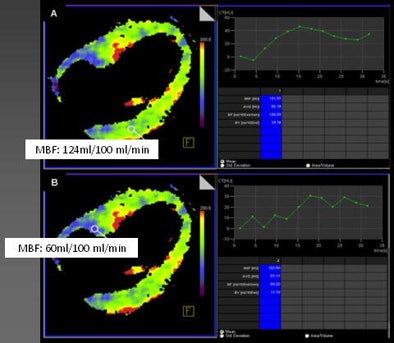
| Semiquantitative analysis: There were significant differences in upslope of signal intensity over time curve between normal and ischemic myocardium both with CT (above) and MRI (below). |
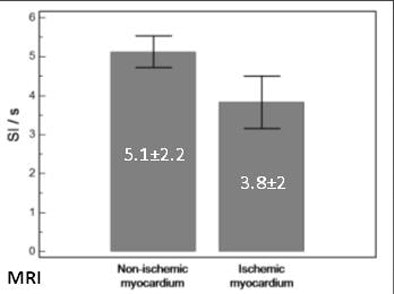 |
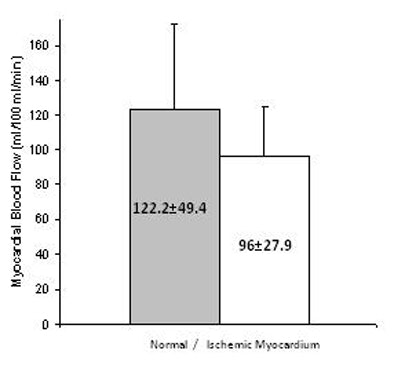 |
| Absolute quantification: Quantitative analysis showed significant differences in myocardial blood flow between normal and hypoperfused myocardium (p < 0.001); moderate correlation between absolute myocardial blood-flow quantification and upslope of signal intensity over time curves (r = 0.47, p < 0.01); and moderate correlation between myocardial blood flow and semiquantitative upslope for hypoperfused and normal myocardium (r = 0.41, p < 0.01 versus r = 0.43, p < 0.01). |
"Adenosine stress dynamic myocardial CT perfusion is, first of all, technically feasible; it can differentiate between healthy and diseased myocardium, it allows evaluation of semiquantitative and quantitative data similarly to MRI, and it seems to be particularly promising for absolute quantification of myocardial blood flow," Weininger said.
The results show that CT is promising for imaging myocardial perfusion, he said.
"CT is not the primary method for the evaluation of the myocardium because its focus is still on the coronary arteries, but considering that CT has potential as an attractive alternative that allows an interpretative assessment of all aspects of the anatomy including function, perfusion, and viability, the question remains when or if CT will become an option for testing," Weininger said.
An audience member asked if there were any issues related to poor temporal resolution owing to the use of shuttle mode, but Weininger said none were apparent, and that, somewhat surprisingly, the color-coding software even worked well in the setting of three-vessel disease.
When comparing CT to other modalities, close is probably good enough, he said. "Missing a tiny perfusion defect on CT would not change treatment if you have identified others on CT," Weininger said.