VIENNA - Vascular imaging in ischemic stroke looks poised to enter an exciting phase.
The optimization of new and more accurate flow-sensitive MR sequences offers the prospect of performing routine high-quality angiographic studies without contrast agents, particularly in patients with chronic renal failure who at present cannot undergo conventional contrast-enhanced examinations. In CT, the development of software platforms capable of differentiating the various components of plaque should assist in analyzing the risk of embolic events.
Atherosclerotic disease of carotid arteries represents the third highest cause of death and the main cause of disability in western countries, and cerebrovascular ischemic events leave 20 million survivors with a permanent disability every year, according to Dr. Carlo Catalano from the department of radiology at University "La Sapienza" Rome. In around 25% of these cases, extracranial carotid artery stenosis can be identified as the main cause of stroke.
CT and MR angiography are fundamental tools for the diagnosis of carotid disease and for the clinical and surgical management of these patients, and he thinks vascular and general radiologists should become more familiar with these techniques for the diagnosis of carotid atherosclerosis.
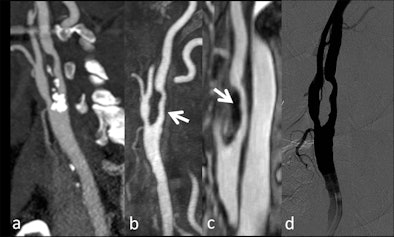 |
| Patient with transient ischemic attack. A: CT angiography depicted a large plaque with a calcified component involving the internal carotid artery; first-pass (B) and high spatial resolution images acquired during the equilibrium phase of an intravascular contrast agent (C) allowed the visualization of the surface irregularities of the soft component of the plaque (arrows). These findings were confirmed by conventional angiographic study (D). (Provided by Prof. Carlo Catalano and Dr. Beatrice Cavallo Marincola) |
"From a technical point of view, the commonest pitfalls are represented by the poor opacification of the arterial vessels, or conversely the superimposition of the venous structures that can cause problems," he noted. "Thus, it's mandatory to use a correct strategy of contrast medium administration that can provide an adequate timing of injection and dose of contrast agent. Moreover, in MR studies, it's important to reach a balance between spatial resolution and acquisition time."
Time-resolved sequences allow the real-time visualization of the contrast medium, which is very useful in diagnosing vascular malformations and fistulas, especially for the analysis of hemodynamic characteristics (feeding arteries and draining vessels) in order to plan the optimal endovascular treatment, commented Catalano. In addition, dynamic sequences may be useful in the evaluation of carotid dissection, and make it possible to visualize abnormal flow dynamics in the false lumen of the affected vessel. Dynamic CT studies are also feasible and can represent a useful addendum to stroke imaging, but these protocols are rarely used in clinical practice because of the high radiation dose, especially if combined with perfusion studies.
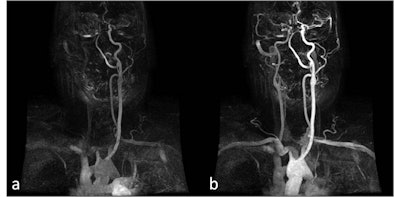 |
| Patient with dissection of brachiocephalic arterial trunk and right common carotid artery. A, B: Time-resolved sequences allow the visualization of an asymmetric transit time of the contrast agent, showing delayed opacification of right common and internal carotid artery compared to the normal left vessels. (Provided by Prof. Carlo Catalano and Dr. Beatrice Cavallo Marincola) |
"In our hospital, we have introduced new CT and MR scanners that feature state-of-the-art angiographic application and sequences, allowing us to perform dynamic and high-resolution studies more easily," he remarked. "Moreover, the recent introduction of high relaxivity and intravascular contrast agents has allowed us to obtain high-resolution images acquired in the equilibrium phase of the circulation, giving an added value in the evaluation of carotid stenosis and plaque morphology. Lastly, the use of dual energy protocols for CT angiography has enabled innovative postprocessing techniques for automated bone subtraction and calcium tagging."
Catalano is the opening speaker at this morning's vascular refresher course. His talk will focus on the technical aspects of state-of-the art imaging in carotid atherosclerosis, giving at the same time major anatomic reminders and several pathologic samples from the clinical arena. He also plans to provide useful information for reporting vascular examinations and the appropriate use of CT and MRI. He wished to acknowledge the contribution of Dr. Beatrice Cavallo Marincola to this lecture.
At the same session, Dr. Luca Valvassori, from the department of neuroradiology, Ospedale Niguarda Ca'Granda, Milan, will speak about vertebrobasilar atherosclerotic arterial disease. His central message is that neurological signs have a vital role to play in the evaluation of vertebrobasilar (VB) atherosclerotic patients, together with the imaging semeiotics of ultrasound, CT, MRI, and digital subtraction angiography (DSA).
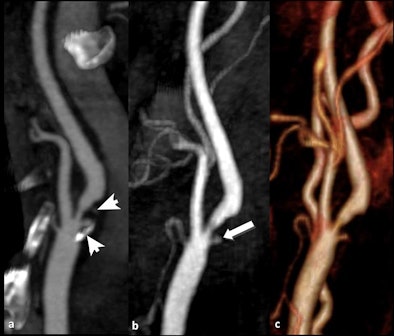 |
| Patient with transient ischemic attack. A: CT angiography depicted a large plaque involving the internal carotid artery characterized by a proximal calcified component and a distal fibrolipidic portion (arrows); first-pass MRI (B) identified a small and deep ulceration of the plaque surface that was partially hidden by calcifications in CT (arrow). C: Volume-rendered reconstruction. (Provided by Prof. Carlo Catalano and Dr. Beatrice Cavallo Marincola) |
"The aim of the presentation is to identify the early imaging semeiotics of vertebrobasilar atherosclerotic disease in order to prevent stroke risk, to direct the clinicians towards the best drug therapy, and to evaluate the indications of endovascular treatment," he noted. "But above all, it is necessary to understand this disease by putting together imaging and clinical signs."
Intracranial atherosclerosis is a systemic and multifactorial disease, associated with atherosclerosis of carotids, coronaries, aorta, and renal and iliofemoral arteries. More than one-third of ischemic strokes occur in the posterior circulation, a leading cause of which is atherosclerotic VB disease. Symptomatic VB disease carries a high annual risk of recurrent stroke, averaging 10% to 15% per year, despite medical therapy, according to Valvassori.
VB stroke is particularly prone to devastating consequences due to the eloquence of the regional brain tissue and is associated with high rates of death and disability. CT angiography and MR angiography are excellent screening tools, but DSA is the gold standard to show focal stenosis, luminal irregularities, thrombosis, occlusion, coronary artery ectasia and elongation, and serpentine aneurysms, and any therapeutic decision requires DSA, he explained. Transient ischemic attack, severe stenosis, and progressive occlusion are the most common signs and symptoms.
An important stroke mechanism in VB atherostenosis is regional hypoperfusion. Both embolic and flow processes can combine to increase stroke risk, reducing the wash-out of emboli from the distal circulation in hypoperfused regions, Valvassori pointed out. Low flow may also promote local thrombus formation at the site of disease, with resultant stroke. Posterior circulation collateral channels, such as the posterior communicating arteries, may maintain adequate distal flow. When evaluated by DSA, the existence and extent of these compensatory blood flow pathways may influence the risk of stroke. Percutaneous angioplasty and stenting for symptomatic atherosclerotic VB stenosis is a feasible, safe, and effective therapeutic method, when drug therapy is not conclusive, he emphasized.
"Any single modality has pros and cons," said Valvassori, who acknowledged the support of his colleague, Dr. Mariangela Piano, based at the same hospital in Milan. "Color Doppler can play a role as well, even if limited to the extracranial portion. CT and MR angiography are very precise for detection of vessel irregularities, stenoses, ectasia, and occlusion. If flow is considered, such as contrast stagnation, collateral circulation, plaque ulceration, and endovascular treatment planning, then DSA is mandatory."
Overall, technological innovations have led to improvements, both in terms of imaging sensitivity and specificity in detection of VB atherosclerotic lesions and of materials for endovascular treatment. The use of state-of-the-art DSA remains fundamental for correct diagnosis, especially in symptomatic patients.
"Preliminary studies indicate that stroke risk in vertebrobasilar disease is strongly related to hemodynamic compromise," he noted. "The improvement of various imaging techniques for assessing cerebrovascular hemodynamic compromise -- using PET, SPECT, perfusion MR and CT imaging, and quantitative MRA -- may provide important correlative and predictive data of stroke risk in order to select criteria for interventional procedures and to define a low-risk population in whom invasive interventions would be unnecessary."




















