VIENNA - Total hip arthroplasty is one of the most effective and rapidly growing orthopedic reconstruction procedures. This means radiologists can expect to see many more hip prosthesis failures over the coming years, but deciding which imaging modality to use to detect them remains problematic. This afternoon's state-of-the-art symposium is designed to address this issue.
There is no easy way to make an early and accurate diagnosis of hip prosthesis failures. Depending upon the surgeon's habits, different diagnostic strategies may be observed, but CT is proving particularly useful for identifying the signs of failures.
"CT has wide indications, as it is more sensitive than radiographs in detecting osteolysis secondary to prosthesis loosening, it clearly shows the periprosthetic fluid collections suggesting infection, and it is the best technique to guide their aspiration for analysis," said Prof. Alain Blum, chief of radiology at Centre Hospitalier Universitaire in Nancy, France.
 |
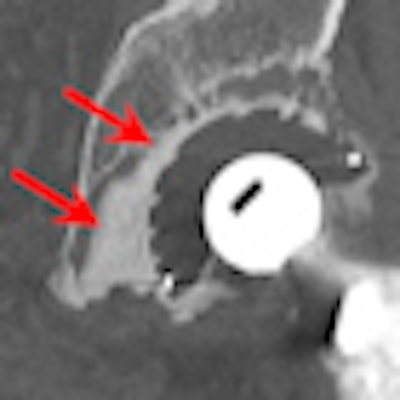
| Acetabular loosening. CT arthrography clearly shows the diffusion of contrast medium around the cement in zones II and III. (Provided by Prof. Alain Blum) |
CT is an important examination for hip arthroplasty patients because it offers another view of not only the prosthesis but also of the bone and all the soft tissues around the prosthesis. It shows the prosthesis components or screw fractures, and demonstrates the contact between the acetabular cup and the iliopsoas muscle in a case of iliopsoas inflammation.
"Because there are some new improvements in CT, such as iterative reconstruction and metal artifact reduction, our analysis of the prosthesis and the surrounding tissues is much, much better today," he noted. "It's an examination that gives us a lot of information. But in all cases, we believe that standard x-rays remain the first test."
To reduce metal artifacts, Blum advises using an x-ray tube of at least 120 kVp, thin-section acquisitions, thicker reconstructions, and a multiplanar reformatting technique along certain planes, along with volumetric rendering. What comes after the x-ray examination, though, depends on the surgeons' habits and preferences, on the radiologists' guidance, and on the available techniques.
 |
| A 55-year-old female patient with a large pelvic collection recurring after drainage, suspected to be related to the hip prosthesis. No infection, no metal, but presence of histamine in the collection. CT arthrography demonstrates the communication between the joint and the collection. (Provided by Prof. Alain Blum) |
"If you have a bad CT scan, you won't have the same algorithm to do the diagnostic strategy," he said. "Again, if you have an MRI machine with the new features, you will probably think differently than if you have an old machine where metal artifacts are too important."
The overriding element, however, appears to be the surgeon's habits.
"Some surgeons say that, for example, if a patient is suffering from hip pain after 10 years and he's wearing a prosthesis, it just means there is loosening of the prosthesis and they don't require any examination to just know there is a loosening," commented Blum. "Someone else will say ‘we have to be sure, we have to be sure there is a loosening, we have to differentiate a septic from an aseptic loosening, we have to look for collections, foot collections, abscesses' ... and the surgeon usually asks for a CT scan if the x-rays don't give the clue."
Typically, a lot of metal artifacts are involved, but usually the results are good and physicians are able to analyze the bone around the prostheses and the soft tissue.
"We are not right now able to analyze all these aspects with MR. ... We still have a lot of artifact," he remarked. "Another point with a CT scan is that we use it to detect impingement between the acetabular component and the thigh muscle. It's a very good technique for that because we know exactly how the acetabular component is located beneath the iliopsoas muscle."
At Centre Hospitalier Universitaire, radiologists perform five CT scans of hip prostheses per week and about two or three CT arthrograms per month because the surgeons prefer CT.
Blum promises to give European Congress of Radiology (ECR) delegates tips to determine when a CT scan should be done versus CT arthrography, which combines the advantages of arthrography and CT.
"There are some previous studies that show arthrography with subtraction is a good technique to detect some loosening and especially acetabular loosening," he stated. "If you combine arthrography with CT, you enhance the formation of those techniques."
He plans to inform attendees about the signs to detect loosening and when they should perform drainage, puncture, or injection of anesthetic or cortical steroid. Lastly, even though it's already been discussed in scientific studies, he'll describe how to perform the CT scan with the best results in order to reduce metal artifacts.
The future for hip arthroplasty will be about the new algorithm to reduce metal artifacts, Blum predicts. "I think all manufacturers will come with the new algorithm for the next RSNA congress," he said. "We are working with Toshiba on that point and consider the fact that in a few months it will really provide new techniques to improve the image quality."
Originally published in ECR Today March 4, 2012.
Copyright © 2012 European Society of Radiology




















