
Computer-aided detection (CAD) technology can be used to help diagnose vertebral body fractures on trauma CT exams, according to research from the U.S. National Institutes of Health (NIH).
A method developed by the NIH team yielded high sensitivity and specificity during testing on 20 trauma patients, showing potential to assist interpreting radiologists as a secondary reader, according to co-author Dr. Joseph Burns, PhD, a former NIH Imaging Sciences Training Program fellow. Burns is currently an associate clinical professor at the University of California, Irvine.
The research was presented by senior author Dr. Ronald Summers, PhD, during a scientific session at RSNA 2012. The software was developed by Jianhua Yao, PhD, with computer programming and data analysis assistance by Hector Muñoz.
Critical concern
Vertebral fractures are a critical concern in blunt trauma cases such as car accidents. There are more than 140,000 vertebral fractures each year in the U.S., according to Summers.
"Rapid and accurate assessment is essential for proper management," he said.
At the same time, radiology practices are dealing with the challenge of larger workloads due to the increasing technical sophistication of CT scanners and declining reimbursement. They also face increasing expectations from the general public and ordering physicians for rapid and error-free image interpretation, Burns told AuntMinnie.com.
Automated, secondary "shadow" readers that scan images in parallel with an interpreting radiologist could be a potential solution to the challenge of assessing large datasets in short time intervals, Burns said. Such a CAD system would be used by the radiologist as an assistant.
Automated detection
The NIH team sought to design and test novel methods for fully automated detection of thoracolumbar spine fractures on trauma CT studies. The approach involves direct detection of the osseous fracture line involvement of the cortical shell of the vertebral body, a task that is accomplished by virtually "unwrapping" the cortical shell, according to the researchers.
After spine segmentation and partitioning is performed, the CAD software segments the vertebral body cortical shell using a deformable dual-surfaces model that takes into account the exterior (periosteal) and interior (endosteal) surface. Next, the cortical shell is "unwrapped" by mapping the 3D cortical shell onto a 2D rectangular space, Summers said.
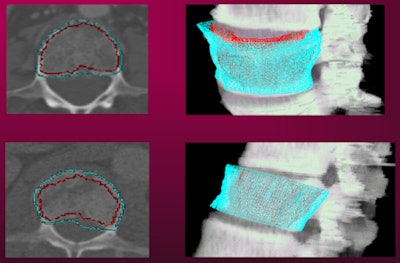 |
| Cortical shell of the vertebral body shown on 2D (left) and 3D views (right). All images courtesy of NIH. |
In the fracture line detection phase, the software detects fracture lines on the unwrapped map, therefore converting a 3D fracture recognition task into a 2D pattern recognition problem similar to road crack detection in computer vision applications, according to the researchers.
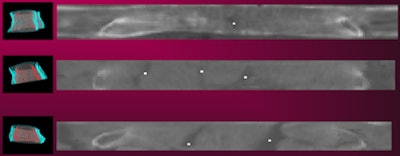 |
| Unwrapped cortical shell map. Dots indicate fracture sites. |
The software extracts 28 features from four categories (associated vertebral body, location, shape, and intensity) from the 2D map and the 3D image. Final classification is then provided.
The researchers evaluated the system on 40 trauma patients (31 men and nine women with a mean age of 41) from 2009 to 2010. Twenty patients, 10 with fractures and 10 without, served as the training set. These cases included 21 distinct fracture sites in 10 fractured vertebrae.
The 20 test patients also included 10 with fractures and 10 without fractures. These cases included 17 fracture sites in 12 fractured vertebrae.
High sensitivity
Free-response receiver operator characteristics (FROC) analysis revealed per-patient sensitivity of 93.6% with 3.2 false positives per patient for the test subjects. The CAD software had per-vertebra sensitivity of 93.5% at 1.7 fractured vertebrae per patient.
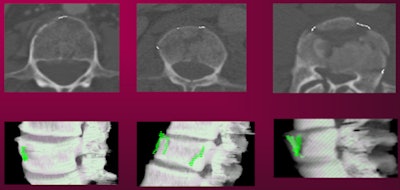 |
| CAD-detected vertebral fractures shown on 2D (top row) and 3D views (bottom row). |
"The CAD system was able to detect and localize vertebral body fractures with low false-positive rates on spine CT studies," Burns said.
In the next phase of the project, the NIH team will try to further develop the technique to detect fractures in the posterior elements of the vertebrae. Although licensing of the software is a possibility, there are no such plans yet, Summers said.
Burns noted that computerized image analysis is not intended to replace radiologist interpretation of imaging studies.
"The intricate thought process complexity and situational plasticity of the human mind allows for recognition of arbitrary, innumerable a priori unexpected pathologies and adaptive image perception for varying geometric perspectives of the same objects," Burns said. "However, CAD can and will be a useful tool in the radiologists' armamentarium, acting as an automated assistant and error checker, designed to analyze images for specific, targeted, high-risk pathologies."





















