VIENNA - General radiologists often shy away from the anatomical complexity of the temporal bone, but Dr. Bert De Foer, from GZA Hospital Sint-Augustinus in Antwerp, Belgium, provides both encouragement and inspiration, noting that he finds this anatomy to be one of the most intriguing regions of the human body.
The hospital conducts around 1,000 CT scans of temporal bone per year and an equal number of MRI examinations, and De Foer spends one and a half days a week imaging the bone.
"It's generally considered one of the most difficult regions of the human body due to subtle details, but once you see through it you will see everything," he said. "I still remember my first intracochlear schwannoma that I missed at university, so you have to know what to look for, and when you know, then you will find it."
De Foer is one of five expert speakers at the head and neck mini course, which begins at 12:30 p.m. today and runs until the final day of ECR 2013. On Monday, he will discuss what, in his experience, are the most appropriate imaging techniques for particular pathologies of the temporal bone region. He will address normal anatomy and pathology, and the highlight will be on routine daily practice pathology. While acknowledging that the temporal bone is relatively complex, he pointed out that once you know what to look for it becomes clear. He recounted his early days of training, learning to how to spot small tumors of the vestibulocochlear nerve.
De Foer will aim to provide insight on the best imaging modalities for examining the temporal bone, depending on the nature of the hearing loss. An ear, nose, and throat surgeon or an audiologist will know if the problem is the result of conductive or sensorineural hearing loss, and this determines which modality should be used.
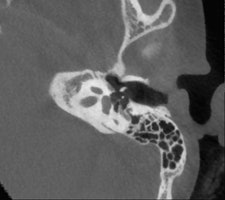
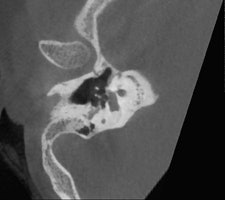 Conebeam CT double oblique reformation of the right temporal bone of a 12-year-old child with conductive hearing loss on the right side, showing a focus of otospongiosis anterior to the footplate. Images courtesy of Dr. Bert De Foer.
Conebeam CT double oblique reformation of the right temporal bone of a 12-year-old child with conductive hearing loss on the right side, showing a focus of otospongiosis anterior to the footplate. Images courtesy of Dr. Bert De Foer."If the problem is related to conductive hearing loss, then it is most likely to be in the middle ear, in the ossicles, and this requires a CT scan or a conebeam CT. But if the hearing loss is sensorineural, you need to use MRI," stated De Foer, adding that the clinical history of the patient and the clinical examination also will help in choosing the appropriate imaging technique.
He is an advocate of conebeam CT, which is growing in popularity, and recounted the advantages of conebeam CT over conventional CT. He said that he previously conducted all temporal bone imaging on a multidetector-row CT, but he now uses conebeam CT far more frequently. It is different because he uses a flat-panel detector, which provides a high resolution, he explained. Images scan at 0.1-mm resolution, whereas multidetector-row CT scans at 0.5 mm to 0.6 mm.
Several of De Foer's patients were initially scanned on multidetector-row CT and returned postsurgery to receive a conebeam CT. The detail on a conebeam CT is much greater, and the dose is also eight to nine times lower with conebeam in our study of it, he said.
De Foer is currently conducting two studies in which he is scoring images of patients imaged by both multidetector-row CT and conebeam CT to compare results of the two modalities.
"The level of detail of the ossicular chain is better. For example, the footplate detail is clearer," he said. "The facial nerve running through the middle ear has a bony coverage which is hardly visible on multidetector CT but is very visible on a cone-beam; likewise, the bony covering of the superior semicircular canal, which is important in the Tullio phenomenon."
De Foer also described how conebeam CT is particularly suitable for otosclerosis. This pathology relates to a demineralization of the bone in the inner ear, which prevents the stapes from conducting sound. Conebeam CT shows this in more detail than multidetector-row CT, especially in the evaluation of the footplate.
 Dr. Alexandra Borges, from the Portuguese Institute of Oncology in Lisbon.
Dr. Alexandra Borges, from the Portuguese Institute of Oncology in Lisbon.
At today's session, Dr. Alexandra Borges, from the Portuguese Institute of Oncology in Lisbon, will present on the anatomy and imaging techniques relevant to pathologies of the oral cavity and salivary glands. She will provide useful tips regarding the choice and tailoring of imaging technique, and will review relevant anatomic relationships underlying the most common patterns of disease spread.
Commenting on the significance of this specialist imaging for general radiologists, Borges said: "Not uncommonly, a clinical examination discloses the tip of the iceberg, whereas imaging unravels crucial information to guide a patient's management."
But to image this region of the body productively, radiologists need to be familiar with the intricate anatomy of the oral cavity, recognize the most common routes of disease spread, tailor imaging studies to specific clinical presentations, and issue meaningful reports answering pertinent clinical questions.
"Imaging may be the only way to assess clinically occult lesions such as the retromolar trigone in patients with trismus and the deep lobe of the parotid gland, therefore having a major impact on their management," she pointed out.
CT and MR are currently the primary imaging modalities to assess the oral cavity. CT is preferred in patients presenting with infectious/inflammatory syndrome. According to Borges, in patients presenting with oral cavity cancer, the use of dental CT software with the acquisition of para-axial and parasagittal high-resolution images in bone algorithm is most valuable in depicting early cortical bone erosion. MRI provides better soft-tissue resolution, and is the first choice in evaluating the deep extent of tumors and for the management of patients presenting with submucosal lesions.
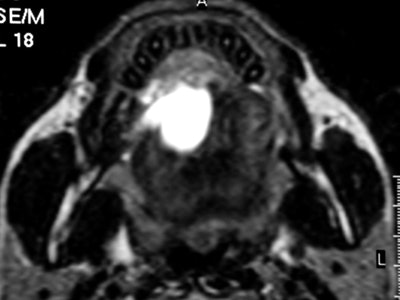 Axial T2-weighted MR image through the floor of the mouth shows a small squamous cell carcinoma (SCC) strategically located in the anterior floor of the mouth. The SCC is obstructing the draining ducts of the sublingual gland with an associated plunging ranula. Image courtesy of Dr. Alexandra Borges.
Axial T2-weighted MR image through the floor of the mouth shows a small squamous cell carcinoma (SCC) strategically located in the anterior floor of the mouth. The SCC is obstructing the draining ducts of the sublingual gland with an associated plunging ranula. Image courtesy of Dr. Alexandra Borges.Referring to the choice of imaging technique, she highlights the importance of considering different patients' specificities. Heavy smokers and drinkers prone to salivary stasis, difficulty in swallowing, and dyspnea are not good candidates for MRI, as this technique is very prone to motion artifacts, and patients with many dental fillings and/or dental implants may do better with MRI than with CT, she explained.
In terms of technical issues to note when imaging the oral cavity, Borges has plenty of good advice. She points out that dental-related artifacts can be avoided by angling the axial sections parallel to the dental fillings on CT or opting for MRI. When lesions are located in the gingival sulcus, jugal or palatal mucosa, or the tongue, cheek puffing is very helpful to clearly depict the full extent of the lesion and separate the lesion from the adjacent mucosal surfaces, she noted.
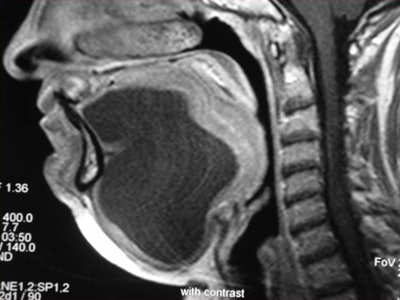 Contrast-enhanced coronal and sagittal T1-weighted images show a large, hourglass-shaped midline cystic lesion in the floor of the mouth splitting the genioglossus muscles. The diagnosis is a dermoid cyst. Images courtesy of Dr. Alexandra Borges.
Contrast-enhanced coronal and sagittal T1-weighted images show a large, hourglass-shaped midline cystic lesion in the floor of the mouth splitting the genioglossus muscles. The diagnosis is a dermoid cyst. Images courtesy of Dr. Alexandra Borges.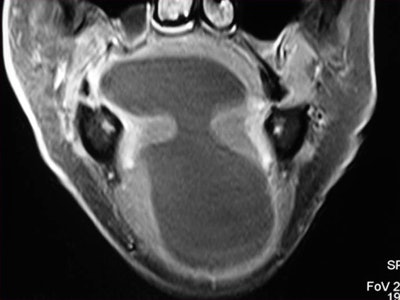
Whenever imaging a malignancy, the full extent of the neck should be imaged for nodal staging. Bone windows are required for all cases of cancer staging and whenever dentomaxillary pathology is suspected.
Finally, she emphasized that when using MRI, it is crucial to instruct a patient not to swallow and to breathe quietly during the entire examination. The use of surface coils can be very helpful for the imaging of superficially located lesions such as the parotid and submandibular glands and the floor of the mouth.
Borges has a wealth of further material to discuss in her 60-minute lunchtime slot. She will also take the opportunity to present the most common pathologic processes as clinical cases, highlighting the main differential diagnoses and the most relevant information that should be included on the imaging report.
Originally published in ECR Today on 7 March 2013.
Copyright © 2013 European Society of Radiology