In a study of more than 300 patients undergoing surveillance after lung cancer surgery, ultralow-dose CT far outperformed chest radiography for detecting cancer recurrence, concluded a study presented this week at the 2013 American Association for Thoracic Surgery (AATS) meeting in Minneapolis.
In fact, CT was more than four times as sensitive as x-ray for detecting recurrence -- finding new lesions early enough to enable repeat resection before the disease could spread beyond the lungs.
"We are finding [cancers] so much earlier now, so instead of waiting two, three, four years, we're finding 96% of the [recurrent] cancers in the first two years," said Dr. Waël Hanna, from the University of Toronto, in an interview with AuntMinnie.com.
Thanks to the National Lung Screening Trial (NLST), there is plenty of data showing that CT is superior to chest radiography for lung cancer screening and follow-up. However, no data compare the two modalities in the setting of patient surveillance after curative resection, said Hanna, who is a thoracic surgery fellow at the university.
Two previous studies looked at standard-dose CT alone for surveillance, and a third study, from France, compared CT to bronchoscopy in lung cancer patients postsurgery, he said.
Nonetheless, x-ray is the modality typically used for follow-up after curative resection for lung cancer; it is performed every three months for the first couple of years, then every six months through the first five years, though things are beginning to change on that front, Hanna said.
"Some organizations like the American Thoracic Society and the National Comprehensive Cancer Network have started to incorporate CT at the discretion of the surgeon because of NLST, but we don't have data," Hanna said. "So that's what our study aimed to show -- that CT is better than x-ray."
After all, ultralow-dose CT's radiation dose isn't much higher than radiography. Ultralow-dose MDCT delivers a radiation dose of just 0.2 mSv, comparable to chest x-ray at 0.16 mSv and lower than standard-dose thoracic CT at about 8 mSv. This enables more frequent imaging with less concern about repeated radiation exposure.
"You don't have to worry about radiation anymore," Hanna said.
Patient enrollment
Between 2007 and 2012, Hanna, along with Dr. Narinder Paul, Dr. Gail Darling, and colleagues, prospectively enrolled 311 patients in the study after curative lung cancer resection. Each patient underwent both surveillance MDCT and chest radiography at three, six, 12, 18, 24, 36, 48, and 60 months after surgery, Hanna said.
CT images were acquired on one of several 64-detector-row scanners of the same model (Aquilion 64, Toshiba Medical Systems) at 120 kVp and 10 mAs, with 500-msec gantry rotation.
Six different radiologists interpreted the images, blinded to the modality they weren't viewing, whether CT or x-ray. When the readers suspected new or recurrent cancer -- "we didn't distinguish them because you have to take them out anyway," Hanna said -- the study team performed standard-dose CT and/or tissue biopsy to confirm the diagnosis.
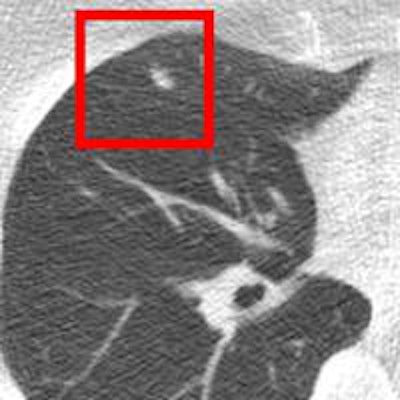
 Lung cancer is clearly visible in the ultralow-dose CT image above but cannot be seen in the chest radiograph of the same patient below. All images courtesy of Dr. Waël Hanna.
Lung cancer is clearly visible in the ultralow-dose CT image above but cannot be seen in the chest radiograph of the same patient below. All images courtesy of Dr. Waël Hanna.
Among the 311 patients enrolled, 1,096 pairs of x-ray and MDCT scans were analyzed, Hanna said. CT was significantly more sensitive than radiography (94% versus 21%, p < 0.0001) for the diagnosis of new or recurrent lung cancer. CT also had a higher negative predictive value than x-ray (99% versus 96%, p = 0.007).
There were new or recurrent lung cancers in 63 patients: 78% were asymptomatic and the cancer was detected only at CT. Two-thirds of these asymptomatic patients were diagnosed within the first year and 26% within the second year, Hanna said.
Two-thirds of the asymptomatic patients were treated with surgery or radiation and had a median survival of 69 months; the rest (12%, 24 of 49) received palliative care and lived a median 25 months.
The researchers used logistic regression and generalized estimating equations to compare diagnostic performance for the two modalities. They used Kaplan-Meier survival and log-rank tests to analyze survival.
"The first landmark finding is that after lung cancer resection, if you follow the patient by minimum-dose CT scan, the patient has a 94% chance that you pick it up versus 21% on x-ray," Hanna said. "For the same radiation dose, you're using a test that can detect cancer at a 94% rate."
Second, the results show that using minimum-dose CT detects 75% of cancers at a time when you can intervene and before they become symptomatic.
"In the past, when we followed them with x-ray, most lung cancer patients came back with recurrent [metastases] to the brain and bones," he said. "Only about 15% had a chance to get reoperated on; they came back too late to do anything. So we've taken the frequency of the second operation up to 75% of patients who had lung cancer again."
MDCT is superior to radiography for follow-up in patients who have undergone curative resection for lung cancer, Hanna concluded, and his department has made the switch in modalities. The study is ongoing, though, so CT would have gone on anyway, he noted.
"We use minimum-dose CT with the same radiation as an x-ray, and we can say whether there's cancer with 94% sensitivity, or more important 99.7% negative predictive value," Hanna said. "So if it's negative, you can look your patient in the eye and say [with 99.7% certainty] you won't have cancer again."