Computer-aided detection (CAD) technology can be an invaluable tool for quantitative diagnosis and treatment planning of craniosynostosis, or premature fusion of skull sutures in infants, researchers from Children's National Medical Center in Washington, DC, have found.
The group has developed an automated system that can label skull anatomy and detect all types of craniosynostosis through a combination of multiple CT imaging features. It can also display skull deformations in a way that may help surgeons manage the condition, said Dr. Nabile Safdar, from Children's National Medical Center and the Sheikh Zayed Institute for Pediatric Surgical Innovation.
"We relied on a new approach that compared individuals to the closest normal case rather than just mean shapes, which could explain improved specificity from approaches others have tried," Safdar told AuntMinnie.com. "Also, we focused heavily on a fully automated system that simplifies use for clinicians."
Safdar presented the research at the recent American Roentgen Ray Society (ARRS) annual meeting in Washington, DC.
Occurring in one in 2,000 births, craniosynostosis leads to abnormal skull shape and ridging and is associated with impaired brain growth and respiratory/visual difficulties. It's classified and treated according to the involved skull suture, Safdar said.
With the exception of metopic craniosynostosis, CT scans are used to diagnose the condition via assessment of suture fusion. Linear measurements are also employed to assess severity.
In addition, caliper measurements are performed and compared with reference standards. Diagnosis is also based on subjective assessment, Safdar added.
Improved diagnosis, treatment
The research team postulated that exhaustive shape analysis of the infant skull could strengthen diagnosis and allow surgery to be better tailored, planned, and optimized (or perhaps avoided altogether).
"Our colleagues in craniofacial surgery said it would be helpful in their surgical planning for craniosynostosis to have more quantitative information about their patients' skull shapes," Safdar said. "Some cases, especially those involving metopic craniosynostosis, can leave quite a bit to the judgment of the surgeon. Improved quantification could reduce variation in diagnosis and surgical technique."
Using a 7° registration procedure that considers only the skull base, the system aligns a subject's cranial bones on thin-slice CT data to a normal skull-shape template (that includes the nasion, posterior clinoid processes of the dorsum sella, frontal bones, parietal bones, occipital bone, and cranial sutures) and determines subject-specific landmarks and deformation fields (Hausdorff distance to the template).
The group studied the method in 57 cases (34 normal, 23 abnormal). The abnormal cases included 11 sagittal synostoses, six left coronal synostoses, and six metopic synostoses.
Significant differences
Significance values for adjacency indices (degree of suture fusion), mean deformations (distance from closest normal reference subject), and mean curvatures (absolute curvature difference with closest point on reference subject) were obtained in all cases on five skull segments and six sutures via Mann-Whitney p-values.
Maximum deformation fields of parietal bones in healthy subjects differed significantly from those in patients with sagittal craniosynostosis, and the parietal bones of those with sagittal craniosynostosis also demonstrated greater deformations than other bones in the same children or in those with metopic synostosis. No significant differences were found between the maximum deformation fields of frontal or occipital bones between healthy subjects and those with metopic or sagittal synostoses.
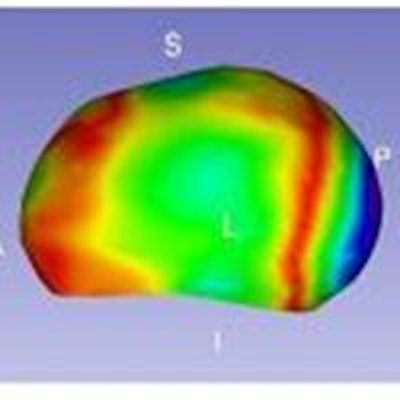
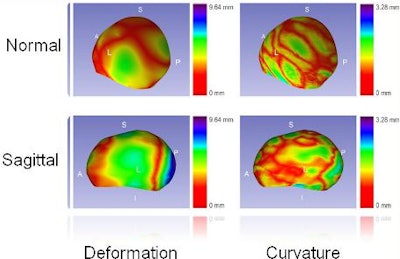 The automated CAD system's ability to display skull deformation and curvature discrepancy demonstrates its potential to better quantify and visualize abnormalities in craniosynostosis. Image courtesy of Dr. Nabile Safdar.
The automated CAD system's ability to display skull deformation and curvature discrepancy demonstrates its potential to better quantify and visualize abnormalities in craniosynostosis. Image courtesy of Dr. Nabile Safdar.The automated CAD system's ability to display skull deformation and curvature discrepancy demonstrates its potential to better quantify and visualize abnormalities in craniosynostosis. Image courtesy of Dr. Nabile Safdar.
For registration of patient images, the system had a mean landmark error range of 2 mm to 4 mm compared with manual landmarks. When compared with manual labeling (separating the skull into its constituent bones), the method had a sensitivity of 0.979 ± 0.038 and sensitivity of 0.996 ± 0.006.
While acknowledging that more clinical validation is needed, the researchers believe that quantifying differences in skull shape will help surgeons be less invasive with their procedures to treat craniosynostosis.
"In some cases, when it's not clear if surgery is warranted, it may provide support for taking a conservative approach and avoid surgery altogether," he said.
In the future, the group plans to validate the tools with more subjects and to develop a surgical planning and simulation platform for surgeons dealing with craniosynostosis. The researchers also hope to apply the methods in a variety of other applications, such as for fractures in other parts of the body, Safdar said.





















