WASHINGTON, DC - Ultralow-dose lung CT with iterative reconstruction looks to be quite robust, but more validation is needed before imaging facilities make it their mainstay, according to a Wednesday talk at the International Symposium on Multidetector-Row CT.
Certainly the use of advanced reconstruction techniques such as model-based iterative reconstruction (MBIR) has fared well in several studies, but whether scans acquired at super-low radiation doses will be good enough for routine use in a wide range of patients has yet to be demonstrated convincingly, according to Dr. Ella Kazerooni from the University of Michigan.
For one thing, images look different at ultralow doses. For another, patient populations vary widely. Third, it's unknown whether the new techniques measure lung nodules as well as standard or low-dose CT. Kazerooni addressed all these issues in her MDCT 2013 presentation.
Good targets for ultralow-dose CT
The lungs are a great target for low-dose and ultralow-dose CT due to the intrinsic high contrast between the air and the lung. This makes it a cinch to extract vessels, segment lungs, and potentially perform diagnostic chest CT at radiation doses at or near those of chest x-ray exposure levels, depending on the clinical indication.
"It may even be that for some types of nodules, ultralow-dose techniques that remove the noise that we've thought of for so long as the 'texture' of the lung on chest CT may make it easier to find and measure ground-glass nodules," said Kazerooni, who is a professor of radiology, director of cardiothoracic radiology, and associate chair for clinical affairs at the university.
"But there may be some trade-offs with respect to quantitative analysis that warrant further investigation," she said.
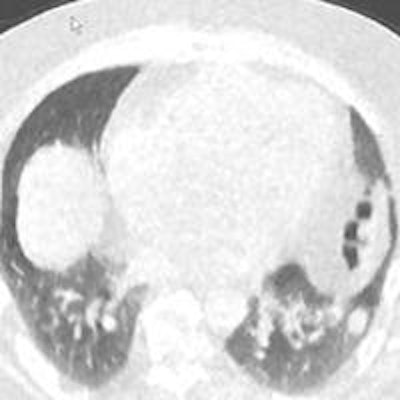
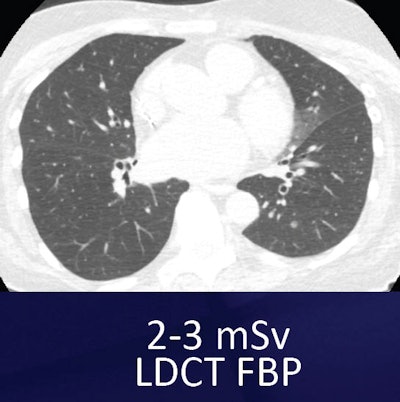 Small nodule in left lung base can be seen both in the standard low-dose filtered back projection (FBP) technique (above) and the ultralow-dose MBIR technique (below). However, the images look inherently different, which may take some getting used to. All images courtesy of Dr. Ella Kazerooni.
Small nodule in left lung base can be seen both in the standard low-dose filtered back projection (FBP) technique (above) and the ultralow-dose MBIR technique (below). However, the images look inherently different, which may take some getting used to. All images courtesy of Dr. Ella Kazerooni.
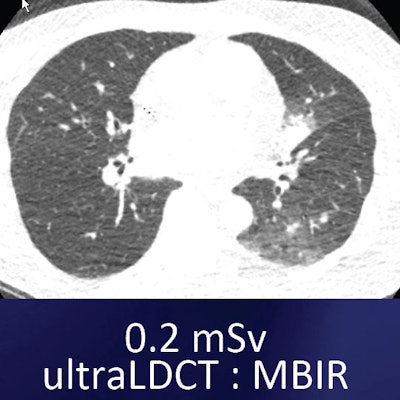
For example, one commercially available MBIR protocol (Veo, GE Healthcare) has shown an impressive ability to reduce noise and improve contrast and spatial resolution, she said. The technique, cleared by the U.S. Food and Drug Administration (FDA) in 2011, uses advanced modeling of system statistics and optics to increase spatial and contrast resolution while permitting vastly lower radiation doses -- as low as 0.2 mSv -- in the lungs.
But no matter how good the reconstruction scheme, ultralow-dose imaging acquisition might be challenged in areas such as near the shoulders, where thicker, denser tissues could potentially create more localized noise and obscure visualization of the lungs, she said. Readers have also noted the blotchy, pixelated appearance of MBIR scans that might make them difficult to read.
"Despite this blotchy, plastic-y, different sort of look to the lung tissue, we can still see quite small pulmonary nodules ... it's just not the pretty picture of yesteryear," she said.
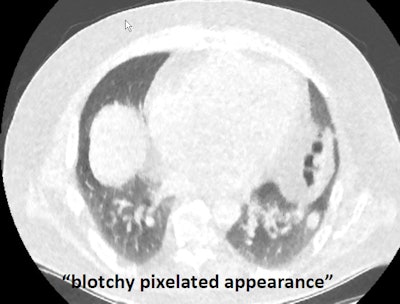 Ultralow-dose CT image of the lungs reconstructed with MBIR looks blotchy and pixelated, but small nodules can still be found.
Ultralow-dose CT image of the lungs reconstructed with MBIR looks blotchy and pixelated, but small nodules can still be found.It's not all about noise and detection; CT must perform a number of functions to be acceptable for lung scans, Kazerooni said. It must detect and characterize nodules and be able to follow them serially over time. Radiologists categorize nodules as solid, part-solid, or ground glass, and CT must permit nodules to be quantified using 2D or 3D techniques.
The question is how iterative reconstruction affects detection and characterization, and a number of papers have attempted to answer it.
Some positive papers
For example, Dr. Yoshitake Yamada and colleagues from the University of Tokyo in 2012 published a comparative study of 100 lung CT scans acquired in 50 patients using both low-dose (4 mGy) and ultralow-dose (0.55 mGy) CT.
The group compared both image noise and subjective image quality for 25-mm axial images, Kazerooni said. They found that image noise was improved using the ultralow-dose technique with MBIR, when compared to the first-generation adaptive statistical iterative reconstruction (ASIR, GE) technique (European Journal of Radiology, December 2012, Vol. 80:12, pp. 4185-4195).
 Dr. Ella Kazerooni from the University of Michigan.
Dr. Ella Kazerooni from the University of Michigan.
In addition, despite the blotchy, pixelated appearance, almost all images were of diagnostic quality, similar to the standard low-dose technique. However, the study did not report on nodule detection.
Another study by Yamada and colleagues used MBIR and ultralow-dose CT in 50 patients, reporting on noise, subjective image quality, and nodule detection for 1.25-mm axial slices (Investigative Radiology, August 2012, Vol. 47:8, pp. 482-489).
Compared with low-dose and ultralow-dose filtered back projection (FBP), ultralow-dose MBIR significantly reduced objective noise (p < 0.01). Still, compared with low-dose FBP, ultralow-dose MBIR and ultralow-dose FBP showed reduced image sharpness (p < 0.001).
The ultralow-dose images were blotchy and pixelated, "however, the performance of [ultralow-dose] MBIR was significantly superior to that of [ultralow-dose] FBP for the detection of noncalcified pulmonary nodules" (p = 0.002) and did not significantly affect screening CT results, according to Yamada and colleagues.
"Using low-dose CT with filtered back projection as truth, ultralow-dose CT detected all of the calcified nodules" 4 mm and larger, Kazerooni said. And when it came to the 184 noncalcified nodules in the study ... the ultralow-dose technique with MBIR picked up more nodules than the ultralow-dose technique with FBP, with a true-positive fraction of 94%, she added. For all nodules 4 mm and larger, ultralow-dose CT picked up nearly 95% of all nodules compared to the reference standard.
Still, the Japanese subjects were smaller than individuals in a typical U.S. cohort, with a mean weight of 56 kg and a body mass index of 22.
"It's important that we validate this in the larger populations that we have in other areas of the world," she said.
Other studies
From Geneva University Hospital, Angeliki Neroladaki and colleagues looked at 42 subjects using standard CT (11 mSv), low-dose CT (2.7 mSv), and ultralow-dose CT (0.2 mSv) with different iterative reconstruction techniques (European Radiology, February 2013, Vol. 23:2, pp. 360-366).
Ultralow-dose CT with MBIR delivered better image quality than ultralow-dose ASIR or FBP; however, it was inferior in the characterization of ground-glass nodules and emphysema, Kazerooni said. The researchers "didn't go into a lot of detail" on the findings, she cautioned, but said the results warrant further investigation.
Finally, in a study presented at the 2012 RSNA meeting, Masaki Katsura and colleagues from the University of Tokyo examined 59 subjects (mean weight, 130 lb) with ultralow-dose CT using MBIR (0.2 mSv), low-dose CT with FBP (4.31 mSv), and low-dose CT with ASIR (0.92 mSv). They found 84 noncalcified nodules 4 mm or larger, 18 ground-glass nodules, and 11 part-solid nodules. There were no significant differences between low-dose ASIR and ultralow-dose MBIR for any nodule type, though detection with the ultralow-dose technique trended higher.
The RSNA study was also very promising, though again in a smaller population, Kazerooni said. All of the studies to date have shown that ultralow-dose CT with MBIR reduces radiation dose substantially and reduces noise to standard low-dose CT levels.
"But we do not yet know the impact on the ability of MBIR to measure the nodule size or to quantify nodules using volumetric studies," she said.
And considering that U.S. obesity rates have climbed 10% to 14% in some states and 25% to 30% in others from 1992 to 2010, "the impact could be substantial, and further study is warranted in our type of patient population to validate these kind of results," Kazerooni said.




















