A new bird flu strain known as influenza H7N9 appeared in China this year and quickly took a number of human victims. An article in Radiology published on Tuesday includes some of the first radiologic images of the effects of the virus, revealing typical patterns of progression and regression on CT scans and radiographs of the chest.
In scans of the 12 infected patients in the study, the most common findings were ground-glass opacities (GGOs), consolidation, air bronchograms, and interlobular septal thickening, with the severity of these features mirroring the severity of the illness at presentation and throughout follow-up, wrote the authors from Shanghai Medical College of Fudan University (Radiology, July 2, 2013).
More deadly than the H1N1 virus that preceded it, H7N9 has killed almost one-third of those hospitalized with the virus. As of June 7, there have been 132 laboratory-confirmed H7N9 infections, and most cases have occurred in middle-aged or older men, according to a World Health Organization report.
Radiological findings
In their study, Dr. Qingle Wang and colleagues aimed to evaluate the radiological findings associated with the H7N9 virus.
"The radiologic imaging examination is essential in the workup," Wang and colleagues wrote. "Chest radiographic examinations are readily available almost anywhere for initial examination and for monitoring disease progression, while the utility and importance of thin-section CT have been well-documented. To our knowledge, the pulmonary radiologic findings in the human infection have not been described so far."
The study included 12 patients (nine men, three women; mean age, 66 years; range, 47-81 years) with novel avian-origin influenza H7N9 virus infection.
All patients presented with fever, with temperatures of 38° C to 40° C, as well as "cough; shortness of breath; and white phlegm and debility at the onset of the disease or within one week," Wang and colleagues wrote. "The patients' conditions rapidly progressed to severe pneumonia and [acute respiratory distress syndrome (ARDS)]."
None raised pigeons or lived near large pigeon populations, though eight had pre-existing conditions ranging from hypertension to diabetes. Also seen in one patient each were rheumatoid arthritis, emphysema, and gout. Four patients reported exhaustion on admission.
All 12 patients underwent chest radiography and thin-section CT, and the investigators examined lesion patterns, distributions, and changes at follow-up CT. Two experienced chest radiologists reviewed the images and clinical data together and diagnosed the findings by consensus. The first images were acquired within one to six days after symptom onset.
Chest radiographs were obtained every one or two days thereafter to monitor disease progression and treatment response, using portable x-ray units. CT was acquired within two to eight days (mean, six days) after the initial x-ray to evaluate progression and possible complications. Noncontrast CT data were acquired on a 16-detector-row scanner using settings of 140 kV, automatic tube current, 0.5-sec rotation time, and inspiration breath-hold. Reconstructions were created using a bone algorithm with 1-mm slice thicknesses and 5-mm intervals.
Opacities at radiography, GGOs at CT
At radiography, the investigators found increased heterogeneous opacity in the lung fields with either a bilateral or unilateral distribution, most commonly affecting the right lower lung (n = 11). Air bronchograms were always seen in the area of consolidation, and the margins were clear when adjacent to the interlobar fissure. Abnormalities could generally be seen within one week after symptom onset; regression in three patients and progression in four corresponded to radiographic results, the authors wrote.
At CT, all patients had lung lesions affecting three or more lobes with a bilateral distribution, but patients were usually affected more on one side than the other, the group reported. The right lung was more affected in seven patients and the left lung in three, with roughly equal distribution in two patients. Extensive GGOs were the most prominent feature, seen in all 12 patients, though some individual lobules were unaffected.
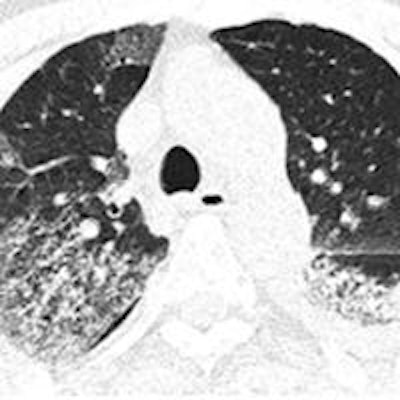
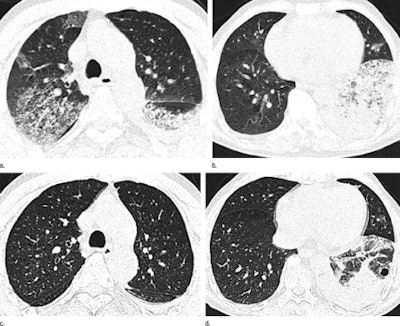 Axial thin-section CT images in 65-year-old man with H7N9 influenza. Top row, initial images obtained at admission show extensive GGOs and consolidation. Bottom row, images at seven-day follow-up show complete resorption of the lesion in the right upper lobe and partial resorption in the left lower lobe with a round cystic change. Images republished with permission of RSNA from Radiology July 2, 2013.
Axial thin-section CT images in 65-year-old man with H7N9 influenza. Top row, initial images obtained at admission show extensive GGOs and consolidation. Bottom row, images at seven-day follow-up show complete resorption of the lesion in the right upper lobe and partial resorption in the left lower lobe with a round cystic change. Images republished with permission of RSNA from Radiology July 2, 2013.Additional findings included consolidations, bronchograms, and interlobular septal thickening (each in 11 patients). Less common were centrilobular nodules (seven patients), cystic changes (four patients), and bronchial dilatation and subpleural linear opacities (each in three patients), Wang and colleagues wrote.
"It is unclear at this time why there was right lower lobe predominance," they wrote. "The phenomenon may be related to the anatomic structure of the trachea and bronchi, as the right bronchus is short and straight, which may facilitate location of the culprit virus. The distribution and rapid progression and GGOs and consolidations with interstitial changes in the H7N9 pneumonia in the current study may help differentiate it from other causes of pneumonia."
Still, the authors cautioned, a specific diagnosis of H7N9 pneumonia could not be made based on imaging features alone.
"Combining imaging features with clinical and laboratory data can help make the early diagnosis of H7N9 infection," they wrote.
Rapidly progressing GGOs and consolidations with air bronchograms and interlobular septal thickening, all with a right lower lobe predominance, are the main imaging findings seen with H7N9 pneumonia, the authors concluded. The severity of these findings corresponded to disease severity at presentation.




















