The search for extracardiac abnormalities detected at coronary CT angiography (CCTA) comes with a major decision that depends, as much as anything, on how hard radiologists really want to look for them, according to a presentation at the recent International Symposium on Multidetector-Row CT.
The choice that imaging professionals face -- full or limited field-of-view reconstruction of thoracic CT images -- can change the number of abnormalities detected, potentially by as much as two-thirds, Dr. Charles S. White said in his presentation at the June meeting in Washington, DC. But full-field reconstruction takes time and effort that is not afforded to other common CT exams. Absent a standard of care, there is no consensus on how to approach the search.
"More than coming down on one side or the other, I just wanted to weigh the arguments," said White, who is director of thoracic imaging at the University of Maryland School of Medicine.
What are we looking for?
Incidental findings are defined as an abnormality identified during an examination obtained for a different indication. Their importance boils down to location and clinical significance of the finding, and they can roughly be divided into three categories:
- Noteworthy but of minimal, if any, significance: small hiatal hernia, vascular anomaly, nodule smaller than 4 mm in a low-risk patient
- Chronic significance: nodules 4 mm and larger, lymphadenopathy
- Acute significance: pulmonary embolism (PE), aortic dissection
"You can draw up your own list of examples, but I think PE and aortic dissection on a cardiac CTA exam are certainly acute emergencies," he said. "Nodules and lymphadenopathies are things that are a little bit more on the chronic side, and things like vascular anomalies, or even a small nodule perhaps in a low-risk patient, would be something you might want to note but you might let pass [based] on things like risk factors."
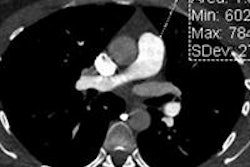
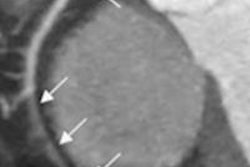
 Acute aortic dissection tops the list of urgent findings requiring immediate care. All images courtesy of Dr. Charles White.
Acute aortic dissection tops the list of urgent findings requiring immediate care. All images courtesy of Dr. Charles White.The locations of extracardiac findings on a typical cardiac CT scan include the aorta and the pulmonary arteries; lymphadenopathy in the mediastinal region; nodules in the lungs, pleura, and chest wall; and abdominal abnormalities, White said.
Study results vary widely
"I've studied some of the studies, and what is denoted as a significant finding differs somewhat because there's a range of values here from 5% to 28%," White said. "Nodules in general are the things most commonly deemed significant, but when you get above 1 cm, the numbers are quite low -- in the 1% to 2% range," he said.
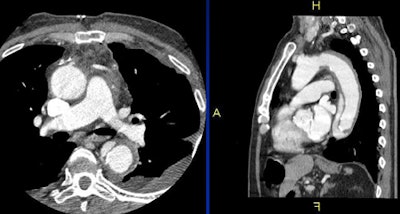
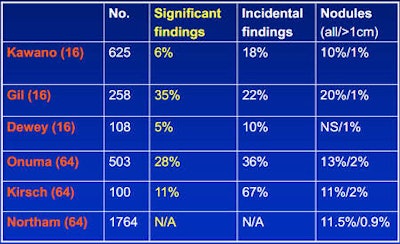 Studies show a wide range of extracardiac findings depending on patient population, criteria for a significant finding, field-of-view, and other factors.
Studies show a wide range of extracardiac findings depending on patient population, criteria for a significant finding, field-of-view, and other factors.Should radiologists use a full or limited field-of-view (FOV)? That is the question -- and it does have an answer -- but there is no consensus among clinicians regarding practice or among the American College of Radiology (ACR) and other societies regarding policy, White said.
For example, a 2008 paper examined the issue and found that only a third of nodules visible on a full FOV reconstruction could be seen using a limited field-of-view.
Viewing cardiac CT scans obtained using only a limited field-of-view "can result in missing more than 67% of nodules larger than 1 cm and more than 80% of nodules smaller than 1 cm," wrote Dr. Meredith Northam and colleagues in the American Journal of Roentgenology in 2008.
Lung nodules are the principal finding that benefits from full FOV reconstructions, White noted, citing a 2010 study in the Journal of Computer Assisted Tomography. Dr. John Fantauzzi and colleagues found that a full FOV approach included 58% (range, 26% to 86%) of the lungs, versus just 14% (range, 8% to 22%) in a limited field-of-view, obviously offering far greater opportunities to detect nodules. But neither captures the entire lung region.
"Even if you include the full field-of-view, the area above the carina is not going to be included, and most lung cancers are in that area," White said.
More to the point, a coronary CTA is not a lung screening exam, he added.
"If you use a restrictive cardiac field-of-view, you do miss a lot of lung, the majority of the lung, but it depends on how restrictive you want to be," he said.
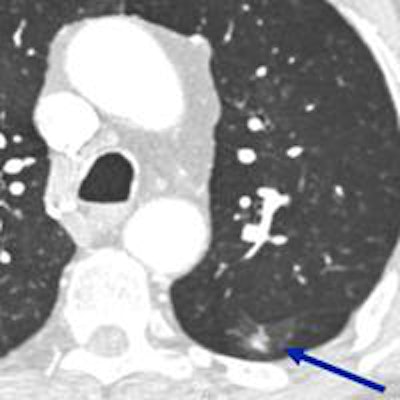
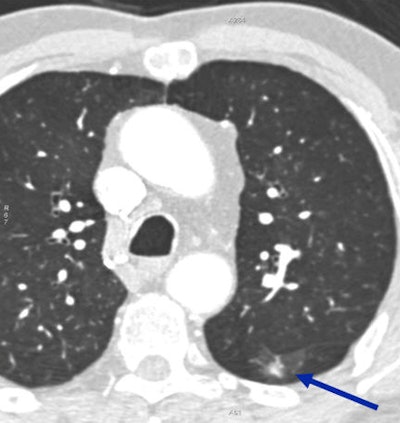 Incidentally detected solid nodule (arrow) turned out to be lung cancer.
Incidentally detected solid nodule (arrow) turned out to be lung cancer.Advocates of the full FOV approach point to the National Lung Screening Trial (NLST), the results of which suggest that the question is applicable to cardiac scans.
"The bottom line is that NLST showed a 20% reduction in mortality among subjects screened for lung cancer, and since nodules are the most common thing you see in an incidental setting, this trial is relevant to a degree," White said.
Those who reject the argument for full field-of-view reconstructions, on the other hand, "say that cardiac patients are a different cohort from lung cancer screening patients, and we don't do full field-of-view reconstructions for other parts of the body, so there's inconsistency," according to White.
And it's true that unlike lung cancer screening subjects, patients undergoing coronary CTA are experiencing chest pain and are symptomatic. They have also been given contrast, and conditions such as pulmonary embolism or aortic dissection that would never be seen at noncontrast lung cancer screening can be identified on CTA. Lung screening subjects also tend to be older than cardiac CT patients.
There is also the question of consistency of practice, White said. Radiologists who specialize in areas such as neuroradiology, spine imaging, or scanning the orbits and ear structures generally limit their search to those narrow anatomic regions. If the whole scanned area has to be examined in cardiac CT scans, one would also have to argue that full FOV reconstructions should be done for all of the other regions as well, "which would represent a complete change of practice," he said. "Whether that's right or wrong is a completely different story. There is no recommendation at the moment by the ACR."
Still, there is evidence of what clinicians do in practice. White's group presented the results of a survey at the 2011 Society of Thoracic Radiology meeting that asked radiologists whether or not they performed secondary reconstructions of the full field-of-view for their cardiac CT exams. Of the 221 respondents, 151 (68.3%) said they did reconstruct using the full field-of-view, whereas 70 (31.7%) said they did not.
"But the literature is all over the place in terms of what they did, so I don't think there is necessarily a settled answer on this," White said. "And while incidental findings are important, I think there are good arguments either way."