
SAN FRANCISCO - A software technique that analyzes CT data to determine the severity of coronary stenosis performed as well as the current gold standard, invasive fractional flow reserve, for detecting ischemia, offering a potentially better and cheaper way to evaluate patients with suspected coronary artery disease, according to a presentation on Wednesday at the Transcatheter Cardiovascular Therapeutics (TCT) annual meeting.
In HeartFlowNXT, a multicenter study performed at 10 centers in Europe, Australia, Canada, and Asia, fractional flow reserve CT (FFR-CT) achieved nearly equivalent sensitivity and significantly higher specificity and positive predictive value for the detection of functionally significant coronary stenosis, when compared with catheter-based FFR or coronary CT angiography alone, the researchers said.
 Dr. Bjarne Nørgaard, PhD, from Aarhus University Hospital.
Dr. Bjarne Nørgaard, PhD, from Aarhus University Hospital.
"In this trial, we compared this test against the gold standard FFR in 254 patients," said Dr. Bjarne Nørgaard, PhD, from the cardiology department of Aarhus University Hospital in Denmark. "What we saw was a significant improvement in accuracy, specificity, and positive predictive value, with no sacrifice in sensitivity and negative predictive value."
The findings suggest that FFR-CT could potentially eliminate the need for risky and costly invasive evaluation and treatment in some patients, especially those at intermediate risk of heart disease -- leading to better clinical outcomes and lower costs, he said.
Evaluating chest pain
Billions of dollars are spent each year in the U.S. to evaluate patients with suspected coronary artery disease -- mostly individuals presenting with chest pain. Current care guidelines recommend that these patients be evaluated noninvasively with tests such as coronary CT angiography (CCTA), SPECT myocardial perfusion, and stress testing before doctors consider invasive evaluation with conventional coronary angiography.
The problem is the poor accuracy of those noninvasive tests; however, there are higher costs and risks associated with catheter angiography for identifying patients with significant ischemia.
"We are very inaccurate in identifying the right patients for invasive testing. Guidelines recommend that we use noninvasive testing, but these are very inaccurate," Nørgaard said, citing a recent study of more than 400,000 angiography patients. Eighty-two percent of the study population had undergone prior noninvasive testing, but invasive angiography revealed that as many as 63% did not have obstructive disease and 39% did not have disease at all.
Fractional flow reserve is an invasive test used in identifying those lesions that should be revascularized. In the invasive version of FFR, a catheter with a small sensor on its tip is threaded to the location of a cardiac lesion and used to measure pressure, temperature, and flow, which can help determine lesion severity. FFR is the ratio of maximum blood flow distal to a stenotic lesion to normal maximum flow in the same vessel.
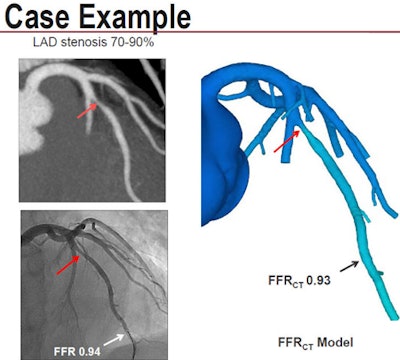 Invasive angiography and CT revealed 70% to 90% stenosis in the left anterior descending (LAD) artery. Conventional FFR and FFR-CT calculated nearly identical flow limitations. Image courtesy of Dr. Bjarne Nørgaard, PhD.
Invasive angiography and CT revealed 70% to 90% stenosis in the left anterior descending (LAD) artery. Conventional FFR and FFR-CT calculated nearly identical flow limitations. Image courtesy of Dr. Bjarne Nørgaard, PhD.Previous research has shown that this approach improves outcomes and reduces costs. "The shortcomings of this test are that it is invasive and pretty costly," Nørgaard said.
On the other hand, the recently introduced FFR-CT analysis is noninvasive; it's based on software (HeartFlow) that creates a 3D model of the coronary tree from CCTA images. It probes it noninvasively to create maps of coronary blood flow based on principles of myocardial mass and resting coronary flow applied to the measurement of vessel size at CT to demonstrate the flow impact of stenosis.
Unlike conventional FFR, FFR-CT is "based on ordinary CT examinations with no modification to imaging protocols, no additional image acquisition, and no additional radiation," Nørgaard said. With current CT technologies for reducing radiation dose, CCTA can be routinely acquired using 1 mSv or less of radiation. And the results really tell you who needs revascularization.
He acknowledged that the FFR-CT process is "a little complicated," requiring supercomputers to process over the course of the day. CT data are uploaded to a laboratory for analysis, and the results are available within 24 hours, Nørgaard said.
Previously, two smaller trials using FFR-CT technology arrived at similar results, but HeartFlowNXT is the first to be significantly powered to evaluate its effectiveness conclusively in multiple centers, he said.
"Moving from CT to FFR-CT, there is a doubling of specificity to 79%, thus reducing the proportion of false-positive results -- that is, CT exams that show significant stenoses that turn out to have little impact on cardiac blood flow," Nørgaard said.
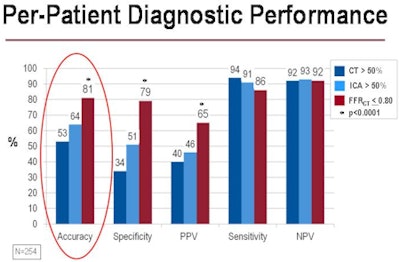 In 254 patients at intermediate risk of coronary artery disease, the use of FFR-CT was equivalent to invasive FFR analysis based on catheter angiography, significantly improving the accuracy, specificity, and positive predictive value of ischemia detection compared to both invasive coronary angiography and CT angiography alone. Image courtesy of Dr. Bjarne Nørgaard, PhD.
In 254 patients at intermediate risk of coronary artery disease, the use of FFR-CT was equivalent to invasive FFR analysis based on catheter angiography, significantly improving the accuracy, specificity, and positive predictive value of ischemia detection compared to both invasive coronary angiography and CT angiography alone. Image courtesy of Dr. Bjarne Nørgaard, PhD.In a population of stable patients with an intermediate risk of coronary artery disease, "we demonstrated high diagnostic accuracy in the detection of ischemia with this new test, FFR-CT, when compared to anatomic interpretation by coronary CT or invasive angiography," Nørgaard said. "FFR-CT leads to a marked increase in accuracy, specificity, and positive predictive value."
Importantly, the FFR-CT technique is performed from standard CCTA datasets without the need of additional imaging, radiation, or medication, Nørgaard said. The results of other noninvasive tests for detecting ischemia -- for example, SPECT and stress echocardiography -- are far less reliable, and SPECT myocardial perfusion imaging delivers a far larger radiation dose than CCTA.
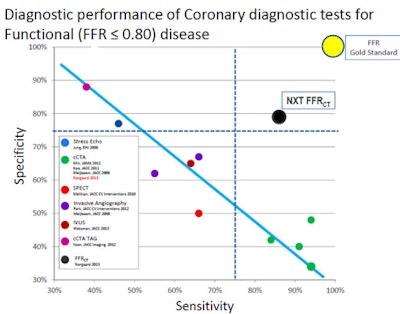 FFR-CT was superior to every diagnostic test except conventional FFR for diagnosing functional disease of the coronary arteries. Image courtesy of Dr. Bjarne Nørgaard, PhD.
FFR-CT was superior to every diagnostic test except conventional FFR for diagnosing functional disease of the coronary arteries. Image courtesy of Dr. Bjarne Nørgaard, PhD.Changing dynamics?
But will the results of HeartFlowNXT really change the dynamics of admitting patients to the cath lab for invasive testing?
It's hard to say because there are so many investigators working on many different ways of determining the significance of stenosis noninvasively, commented panelist Dr. Bernard Gersh, from the Mayo Clinic in Rochester, MN. Nevertheless, the current study is an important one with the potential to affect clinical practice.
"What's going to be interesting is what it will do to our conventional methods of stress testing," Gersh said.
 Session panelists (left to right): Dr. David Erlinge, Dr. Philippe Généreux, Dr. Bernard Gersh, and Dr. James Hermiller.
Session panelists (left to right): Dr. David Erlinge, Dr. Philippe Généreux, Dr. Bernard Gersh, and Dr. James Hermiller.The results are especially important considering the current lack of alternatives for combining anatomic and functional testing to assess the severity of stenosis, said Dr. Philippe Généreux, from Hôpital du Sacré-Coeur de Montréal, during a panel discussion at the TCT show to discuss the results.
"I think this study brings a breath of fresh air to noninvasive testing, and the real question will be on what subset of the population we should use this new technology," he said.
"We need more specificity in our screening studies, and the beauty of this study was that there was much greater specificity, but there wasn't much price to be paid in sensitivity -- you get the best of both worlds with this," said panelist Dr. James Hermiller, from St. Vincent Heart Center of Indiana.
Still, Hermiller cautioned, "I think anything you do is going to require a good cost-outcome analysis, and we need to compare it to people who undergo SPECT exercise and the false positives that go along with that, and the total cost of cathing people who don't have significant lesions."
The study is a "big step forward," commented Dr. James Min, from Weill Cornell Medical College and NewYork-Presbyterian Hospital. What separates HeartFlowNXT from previous FFR-CT trials is, first of all, its comparison of FFR-CT with CT-based estimates of stenosis, and CT was performed using optimal methods in strict adherence to societal guidelines.
"Second I think [the software] represents a new iteration of the technology" of measuring flow dynamics, a science that has improved substantially over time, Min said.




















