The use of 3D reconstruction along with CT imaging is quite common for many types of exams performed by radiology practices. In some cases, it is a minimum requirement in order to bill for the exam that was intended, while in other cases it will garner extra reimbursement.
Either way, 3D reconstruction must be specifically documented for coders to properly bill for the procedures. In this article, we will review the financial reasons for providing good documentation, identify when 3D reconstruction is required and when it is an additional charge, and explore the documentation requirements that will provide the maximum reimbursement in these various circumstances.
CT angiography (CTA) has always required angiographic reconstruction, which today implies 3D (not 2D) reconstruction, according to the American College of Radiology (ACR). Failure to perform or document the 3D reconstruction that is a component of a CTA will result in lower reimbursement as an ordinary CT scan rather than the intended CTA procedure.
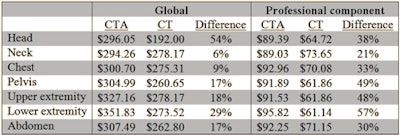
The following table gives an example of the financial benefit of including the proper documentation to receive the correct reimbursement (or, conversely, the penalty for not properly documenting).
 Difference in reimbursement for CTA versus CT. The table uses the Medicare national payment level as of July 2015.
Difference in reimbursement for CTA versus CT. The table uses the Medicare national payment level as of July 2015.When radiologists fail to adequately document a CTA of the head, they will lose 38% of their professional component reimbursement if the exam is coded as a CT head scan with contrast. In the imaging center, the combined loss would be 54% of the reimbursement.
So, it pays to know the rules of documentation and follow them.
Because managed care payors usually require prior authorization for CT exams, it's important for the final billing to match the requested exam. When a CTA is requested and precertified, billing for an ordinary CT with contrast will create a mismatch and might result in no payment at all unless the claim can be successfully appealed. This process requires time and effort that can be avoided by providing thorough documentation to match the exam being performed.
Billing for 3D reconstruction related to other exams is a bit trickier, but when the circumstances warrant its use there will be additional reimbursement as a result. Under Medicare regulations, 3D reconstruction may only be billed if an initial study shows an abnormality that requires additional rendering using 3D reconstruction.
Most managed care payors are following the Medicare guidelines in this regard. The presence of the following diagnoses will justify the medical necessity of the 3D reconstruction without any secondary diagnosis, and they should be specified in the initial documentation of the exam:
- Paralysis agitans
- Essential and other specified forms of tremor
- Genetic torsion dystonia
- Spasmodic torticollis
- Other fragments of torsion dystonia
In some cases, a secondary diagnosis will justify the use of 3D reconstruction for additional reimbursement. Secondary diagnoses that are covered include nonspecific or abnormal findings in the original exam of the following areas:
- Skull and head
- Lung field
- Other intrathoracic organs
- Gastrointestinal tract
- Genitourinary organs
- Abdominal area, including the retroperitoneum
- Musculoskeletal system
A written request for the 3D reconstruction must be included in the medical record. This order can come from the radiologist for inpatient exams, although in outpatient settings, such as an imaging center or independent diagnostic testing facility (IDTF), a referring physician's order must be obtained.
Additional prior authorization from a managed care payor might also be needed to ensure reimbursement for the additional 3D reconstruction. The regulations require documentation of concurrent physician participation, which means active participation in and monitoring of the reconstruction process, including the following:
- Design of the anatomic region that is to be reconstructed
- Determination of the tissue types and actual structures to be displayed
- Determination of the images that are to be archived
- Monitoring and adjustment of 3D work product
Whenever 3D reconstruction is performed, whether integral to CTA or as an addition to an abnormal exam, ACR says to clearly document the rendering and interpretation of the images, either as a separate report or in a distinct section of the basic service report.
Adequate documentation includes the following:
- Whether or not an independent workstation was utilized; this is a key element that allows the coders to use the correct coding
- Which techniques were used, such as:
- Maximum intensity projection (MIP)
- Shaded surface rendering
- Volume rendering
- What the 3D rendering showed, independent of the original exam
When a separate report is issued, the location and time of the original exam should be included, especially if the reconstruction is performed from a different facility. ACR also recommends that an archive of the reformatted images be retained as part of the permanent record of the study using the same guidelines as for retention of any other study.
Medicare's recovery audit contractors (RACs) are on the lookout for 3D reconstruction billing that does not meet the standards to support medical necessity. Adherence to the requirements for ordering and documenting 3D exams will avoid any appearance of improper billing practices, even if reimbursement for the additional 3D imaging is denied by certain payors.
Radiology practices might want to consider creating templates that ensure that guidelines are followed for each and every 3D case. This makes it easier for radiologists to become used to providing full and complete documentation as a regular part of their routines, thus helping to improve the potential to maximize practice reimbursement.
Carin Carlson is vice president of business development at Healthcare Administrative Partners (HAP), where she is responsible for all new business activity, including sales, marketing, product development, and strategic planning.
The comments and observations expressed herein are those of the author and do not necessarily reflect the opinions of AuntMinnie.com.




















