Initial CT findings in patients suspected of having appendicitis are a largely untapped source for predicting hospital costs and resource utilization down the line, according to a new study in the September issue of the American Journal of Roentgenology.
Researchers from NYU Langone Medical Center examined initial CT scans in 138 patients presenting with suspected appendicitis. They noted several CT findings -- from wall thickness to fluid collection -- that accurately predicted the need for inpatient surgery and even the length and expense of hospital stays.
In the era of heightened vigilance over healthcare costs, admission CT findings "serve as independent predictors of hospital resource utilization in suspected acute appendicitis," wrote Dr. Neal Viradia, Dr. Andrew Rosenkrantz, and colleagues (AJR, September 2015, Vol. 205:3, pp. W275-W282).
Cost takes center stage
Along with helping to insure more patients, a key aim of the U.S. Patient Protection and Affordable Care Act has been to reduce healthcare costs by restructuring the payment system for doctors and hospitals. Because initial imaging exams are indicated for a wide array of conditions, baseline imaging studies have an important role in predicting and shaping resource utilization.
The relationship between early imaging and costs may allow the creation of models to predict specific aspects of resource utilization, such as inpatient costs and hospital length of stay, the authors wrote.
"We showed that a variety of imaging findings predicted these outcomes independent of other standard factors such as patient demographics, comorbidities, white [blood cell] count, and payor status," said Rosenkrantz, an associate professor of radiology, in an interview with AuntMinnie.com.
Previous studies have associated specific imaging findings with clinical outcomes, but Rosenkrantz said they have not provided comprehensive models for initial CT of acute appendicitis.
The study included 138 patients (76 men, 62 women; mean age, 40 ± 21 years) who underwent baseline CT after being admitted for suspected acute appendicitis. The researchers used linear and logistic regression to identify independent predictors of resource utilization from the viewpoints of both payor and hospital.
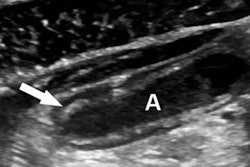
A radiologist reviewed CT data for appendiceal-related findings and noted the presence or absence of appendicoliths, periappendiceal free fluid, periappendiceal fat stranding, loculated right lower quadrant fluid collection, and extraluminal free air.
CT predicts outcomes, costs
The results showed that nearly three-fourths (70.3%, 97/138) of the patients underwent inpatient surgery, which was most often performed the same day as CT (53/97) or the day after imaging (38/97). The authors noted that 91.8% (89/97) of the surgeries were performed laparoscopically, with the rest using an open approach.
Multivariable analysis revealed several significant independent predictors of whether a patient would undergo inpatient surgery:
- Greater age (p = 0.029)
- Lower Charlson comorbidity index (CCI) (p < 0.001)
- Smaller appendiceal wall thickness (p = 0.004)
- Absence of loculated right lower quadrant fluid collection (p = 0.006)
- Absence of periappendiceal free fluid (p = 0.018)
Together, these factors had a sensitivity of 92.7% (89/96) and specificity of 65.8% (25/38).
An additional 22 patients had surgery for appendicitis after discharge, resulting in a total of 84.1% (116) undergoing surgery. Among these patients, pathological assessment showed acute appendicitis in 97.4% and complicated appendicitis in 56.9%, the authors wrote.
The mean length of hospital stay was 2.8 ± 2.9 days (range, 1-17 days; median, 2 days), with almost half (48.6%) of patients discharged on the day of admission.
According to the multivariable analysis, the following were significant independent predictors of same-day discharge, collectively producing a sensitivity of 79.1% and specificity of 64.2%:
- Smaller appendiceal diameter (p = 0.003)
- Absence of periappendiceal free fluid (p = 0.010)
- Laparoscopic surgery (p = 0.003)
Patients not treated surgically were managed via drain placement or with antibiotics, Rosenkrantz and colleagues wrote.
In all, 29.7% (41/138) of patients underwent repeat abdominopelvic CT scans. Significant predictors of repeat imaging had a sensitivity of 82.5% and specificity of 68.1% and were as follows:
- Greater CCI (p < 0.001)
- Greater appendiceal wall thickness (p = 0.005)
- Presence of periappendiceal free fluid (p = 0.016)
Finally, 9.4% (13/138) of patients had a subsequent emergency department visit within 30 days. The only significant predictor for this event was the presence of an appendicolith, with a sensitivity of 61.5% and specificity of 68.8%. Eight percent of patients (11/138) had a repeat inpatient hospitalization for abdominal pain within 30 days.
The mean total inpatient costs were $19,120 ± $13,422 (range, $3,606-$90,382; median, $14,482). The following were significant independent predictors of greater inpatient costs:
- Greater appendiceal diameter (p = 0.003)
- Presence of free air (p = 0.033)
Costs rose much more rapidly with increasing appendiceal diameter in the presence of free air, the authors wrote. In patients without free air and an appendiceal diameter of 6-27 mm, costs were predicted by the formula $8,047.16 + ($745.02 x appendiceal diameter). In patients with free air and an appendiceal diameter of 11-19 mm, costs were predicted by the formula $-39,261 + ($4,425.84 x appendiceal diameter).
These two factors together accounted for just 14.5% of the total cost variation; however, costs were poorly predicted when they exceeded $45,000 and better predicted when they fell below it.
Model accounts for most patients
The few high-cost patients are where the cost method failed, Rosenkrantz said.
"We were able to develop an interesting model for the bulk of patients, but the model didn't perform as well for admissions that [reached] particularly high costs -- the outliers, so to speak," he said. "This suggested that there is a subset of admissions that for reasons not apparent through our analysis generated very high costs relative to other patients in the cohort."
Overall, the study revealed a number of CT findings that served as independent predictors of several measures of downstream utilization, the authors wrote. Facilities can use them to optimize their own resource utilization.
"A hospital, for instance, could use a model for evaluating their own internal resource utilization and evaluate their own practice patterns for this disease process to identify potential areas for optimization at the hospital level," Rosenkrantz said, cautioning that the model isn't necessarily predictive at the patient level.
"This may provide an example that investigators in other areas could apply to develop similar models for other disease entities," he said. "The possibilities could be numerous in conditions for which imaging is routinely obtained in a standardized fashion early in the patient's evaluation."
Trauma and stroke come to mind as potential candidates for modeling, but maybe not coronary artery disease, because in many facilities patients do not routinely undergo initial noninvasive imaging at admission, Rosenkrantz added.