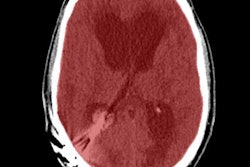
For ischemic stroke patients who are candidates for revascularization, CT perfusion imaging is more important for successful revascularization than the length of time from symptom onset, according to a study presented this week at the American Heart Association's (AHA) International Stroke Conference.
In a study of 102 ischemic stroke patients who had endovascular therapy, researchers found that when perfusion imaging is performed, large areas of brain tissue can be safely salvaged up to 18 hours after stroke symptoms begin. The time limits were thought to be much more limited.
"Using this image-based selection, we would be able to look at any patient who comes through the door to identify the ones likely to benefit from these therapies, regardless of what the clock shows," said author Dr. Jenny Tsai, a neuroimaging and vascular neurology fellow at the Stanford Stroke Center, in a statement. "This is important because we want to offer the best treatments to every patient who suffers stroke and who may benefit from them."
Endovascular treatment to mechanically remove the clot blocking blood flow to the brain works best when performed within six hours of symptom onset, while drug treatment is best within 4.5 hours, the authors noted.
But the study showed good results even in patients who had long exceeded the recommended limits of time since symptom onset. Good recovery with little or no disability was achieved in 71.4% of patients treated within six hours and in 61.7% of patients treated more than six hours after stroke onset, the group reported.
In fact, there was no significant association between time to treatment and good outcomes when CT perfusion imaging showed salvageable brain tissue, according to the researchers. The two-year study, called CT Perfusion to Predict Response to Recanalization in Ischemic Stroke Project (CRISP), used CT perfusion to identify adult acute stroke patients who were likely to benefit from endovascular therapy. It was funded by the U.S. National Institutes of Health (NIH) and was conducted at six U.S. sites.
"We now have a very effective treatment for the large and disabling acute strokes," Tsai said. "And we know that there are patients likely to benefit from interventional treatments who are not being captured using basic imaging and time criteria alone. We need to do better."