SAN FRANCISCO - A little over a year after Medicare payments were approved for CT lung cancer screening, practices are finding the support they need to do it properly, according to a May 13 talk at the American Thoracic Society annual meeting (ATS 2016).
There is now agreement for what constitutes a positive screen and how nodules should be managed, thanks to the Lung-RADS reporting system introduced in 2014. There is support for determining how well screening programs are doing in terms of patient outcomes, thanks to the American College of Radiology (ACR) registry that is starting to collect meaningful data.
And there is support for radiologists doing a task that is potentially of great benefit to society, as well as to their own profile with patients, according to Dr. Ella Kazerooni, director of cardiothoracic radiology at the University of Michigan and chair of the ACR's committee on lung cancer screening.
"Lung cancer screening -- I see it for radiologists as a way to come out of the closet of those dark reading rooms and to make a bigger difference," she told ATS 2016 attendees.
Cut mortality, boost survival
CT lung screening programs are helping radiologists find early-stage lung cancer, as well as other conditions such as chronic obstructive pulmonary disease (COPD) that significantly affect morbidity and mortality.
"With the three leading causes of death in the U.S. being all in the thorax -- cardiovascular disease, COPD, pneumonia/infection -- and lung cancer as a leading cause of cancer death, there's a tremendous opportunity to make a difference," she said.
 Dr. Ella Kazerooni from the University of Michigan.
Dr. Ella Kazerooni from the University of Michigan.The 2011 National Lung Screening Trial (NLST) showed that screening works, demonstrating a 20% reduction in lung cancer mortality and a 6.9% reduction in all-cause mortality. The study showed it takes about 320 lung cancer screenings to save a life, Kazerooni said.
Later work showed that screening is cost-effective, with a cost of about $81,000 for a quality-adjusted life year (QALY), a number that can vary based on how screening is implemented. For example, costs can be reduced significantly by increasing the nodule size used to define a positive scan, from the current 4 mm to 5 mm or 6 mm.
Final approval for CT lung cancer screening from the U.S. Centers for Medicare and Medicaid Services (CMS) in February 2015 came with a mandate for shared decision-making with the patient, something that radiology has never experienced and which remains poorly understood, Kazerooni said. Doctors thought they were already sharing decisions when they spoke with their patients about a test.
Still, no one is sure how to optimize the process, whether patients want it, or if it makes a difference. Shared decision-making is generating a lot of discussion and questions now, she said.
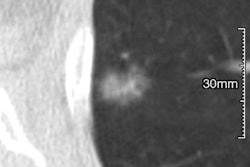
Also, one problem with screening is that lung nodules are everywhere, and most adults have them.
"With better scanners and higher resolution that has happened over the past 30 years, you get more of these pesky little nodules," she said. In some places, such as the "histoplasmosis belt" of the central U.S., nodules have become a normal part of the process for most screening subjects.
Lung-RADS, ACR registry are born
To make sense of myriad findings and implement a common lexicon and practice model, the ACR developed Lung-RADS, a standardized nodule identification, classification, and reporting system. It remains the only CMS-approved nodule classification system.
Another key piece of screening, the ACR Lung Cancer Screening Registry, was developed to monitor results and patient outcomes of the screening program. To date, it is the only CMS-approved registry for lung cancer screening, and participation is required for reimbursement.
Because the ACR registry requires the use of Lung-RADS, both Lung-RADS and the ACR registry are required to be paid for lung cancer screening.
"It's both a positive and a negative to have federal requirements driving direction, but in this case, it allows us to move forward together instead of having six or 10 different reporting schemes and management tools," she said.
Working with all of the societies to develop a lung cancer screening model, the fundamental question raised was whether screening in practice would perform the same way it does in clinical trials, Kazerooni said.
Payors, the public, and different providers want to know if screening does more good than harm, whether shared decision-making helps, whether programs should offer smoking cessation, whether they are maintaining low radiation doses, and whether screening is being performed appropriately to minimize complications and reduce mortality.
"If you're not looking, how do you know?" Kazerooni asked. "And that was really the driver behind the CMS requirement for a registry. How do we know ... that we're actually doing more benefit than harm?"
It took some thought to get to the place where Lung-RADS is today, she said. In NLST, 40% of individuals had a false-positive scan using a threshold of 4 mm as a positive screen, and that rate had to be reduced.
Lung-RADS was advanced by Pinsky and colleagues, who last year analyzed results of the International Early Lung Cancer Action Program (I-ELCAP). They found that raising the nodule size threshold reduced follow-ups substantially without producing delays in cancer care, and these findings were used to inform Lung-RADS, Kazerooni said.
In an analysis of 21,000 I-ELCAP subjects, for example, the group found that just raising the nodule size threshold from 5 mm to 6 mm reduced the positive screen rate from 16% to 10.2%, cutting workup by 36%. The reduction came with no delay in cancer diagnosis, which appeared only at higher nodule-size thresholds.
As for nodule size, "this is a question we're going to keep having to come back to," Kazerooni said. What's clear is that if the size threshold is increased, "you can reduce positive screens, anxiety, and downstream diagnostic testing complications, with the goal of not missing cancer by going too high."
Histology also plays a big role in Lung-RADS recommendations. For example, minimally invasive adenocarcinomas have the highest likelihood of being cancer, while the cancer rate of pure ground-glass nodules is very low.
Thus, size and the adenocarcinoma spectrum of ground-glass nodules form the basis of Lung-RADS' 0 to 4 classification system, she said. Zero is an incomplete scan, 1 is negative, 2 is benign-appearing, 3 is probably benign, and 4A and 4B represent different levels of suspicious nodules.
Two important modifiers to this scheme include "S" for clinically significant nonlung cancer diagnoses, such as aortic aneurysms and thyroid masses, and "C" for a patient with prior lung cancer returning to screening.
The ACR began backing away from the "C" modifier due to a reimbursement problem for patients, who are no longer eligible for "screening" when they turn 77.
But Lung-RADS does improve screening efficiency, according to several studies. Last year Pinsky, Kazerooni, and colleagues showed that applying Lung-RADS to NLST results would cut baseline positive scans from 26.6% at NLST to 12.9%. Meanwhile, sensitivity fell only slightly, from 93.8% to 86.1%, and positive predictive value almost doubled, from 3.8% to 6.9%.
Early registry results show that radiologists are doing an excellent job with radiation dose, she said. And they are being used to hone follow-up recommendations, including the Fleischner guidelines.
A few problems are cropping up as CT lung cancer screening advances, however. Insurers are now pressuring patients to visit cheaper imaging centers for their annual follow-up scans rather than the expert institution where they started, apparently mindless of the need for expert readers and consistency in the process, Kazerooni said.