A new analysis of screening intervals for CT colonography (CTC) found that it may be safe to wait as long as five to 10 years to screen again after an initial negative scan. The results are good news for the cost-effectiveness profile of CTC, investigators report in Radiology.
The group from the University of Wisconsin-Madison analyzed results from 1,429 patients who returned for repeat screening CTC more than five years, on average, after their initial negative CTC exam. They compared the CTC findings at follow-up with the initial screening and found fewer advanced lesions and just two small cancers in the cohort (Radiology, August 22, 2016).
The results support the five- to 10-year screening interval for CTC suggested in the 2005 CT Colonography Reporting and Data System (C-RADS) recommendations, lead author and professor of radiology Dr. Perry Pickhardt wrote in an email. "Going beyond five years further improves cost-effectiveness," he added.
CTC follow-up needs unclear
Although CTC is well-validated for an initial round of screening, little is known about its use for repeat screening after an initial negative colonoscopy.
Thankfully, enough follow-up CT colonography screens have been performed over time to formally assess specific colorectal findings, the authors wrote. The current study aimed to determine the rate and types of polyps detected at repeat CTC screening after an initial negative screen.
In its 2005 C-RADS recommendations, the American College of Radiology's CT Colonography Working Group recommended repeat screening with CTC every five to 10 years. Other groups have settled on a five-year recommended follow-up, but without explanation.
Mostly healthy patients
The initial population of 5,640 asymptomatic adults underwent CTC screening at a single center between 2004 and 2010 and received a negative result (no polyp ≥ 6 mm). By May of 2016, 1,429 of them (25%; mean age, 61.4 years) had undergone repeat CTC screening, the authors wrote.
Pickhardt and colleagues Dr. Dustin Pooler, Dr. Ifeanyi Mbah, Dr. Jennifer Weiss, and Dr. David Kim analyzed the results of all patients who had positive findings at follow-up, comparing them with the initial CTC results. Positive findings were defined as polyps 6 mm or larger, a threshold that typically requires follow-up.
At follow-up CTC, the percentage of patients with positive results (12.1%) was lower than the percentage of patients (14.3%) who were positive on initial screening.
"The interval cancer rate at routine CT colonography surveillance was lower than the cancer rate seen at initial screening, as well as the reported interval rates at [optical colonoscopy]," the team wrote.
In other results, the researchers found that large polyps were less common on subsequent screening rounds, with a prevalence of 3.8% on follow-up rounds versus 5.2% on initial screening (p = 0.02). The rate of advanced neoplasia (advanced adenomas and cancer) at follow-up was 2.8%, compared with 3.2% at initial screening (p = 0.52), and the rate of invasive cancer was 0.14% versus 0.45% (p = 0.17). The drop in prevalence was greatest among the more clinically relevant lesions.
"We only identified two localized colon cancers, one that appeared to be a de novo growth 10 years after initial CT colonography screening and another that progressed over five years from a flat 13-mm lesion," they wrote.
Optical colonoscopy misses lesions
Among the 173 patients with positive findings at CTC follow-up, 122 (71%) underwent optical colonoscopy for confirmation and possible resection, while the rest, especially those with small polyps (C-RADS Category C2), were enrolled in surveillance.
In this group of 122 patients, 161 lesions were identified, and 87% of them were confirmed and resected. The remaining 21 lesions (13%) were not found at subsequent optical colonoscopy, representing either CTC false-positive or optical colonoscopy false-negative findings.
Among 42 total advanced lesions seen at follow-up, 33 (78.6%) were right-sided and 22 (52.4%) were flat, compared with 45.4% right-sided (p < 0.001) and 11.3% flat lesions (p < 0.001) at initial screening.
"Improved recognition of flat lesions ... appears to be the most important difference between our initial and repeat CT colonography screening rounds," the authors wrote. "Not only does each flat lesion missed at initial CT colonography lower the first-round prevalence, but detecting them at repeat screening further increases the positive rate at the second round."
The screening subjects were also five to 10 years older at the second round, probably also contributing to the higher overall polyp prevalence at follow-up.
Large right-sided serrated lesions were also more prevalent at follow-up, with a detection rate of 1.4%, compared with 0.5% (p < 0.001) at initial screening, Pickhardt and colleagues wrote.
For bowel preps that use only an iodinated oral contrast material or no contrast at all, the detection rate for flat lesions is probably still reduced, they cautioned.
But while flat-lesion detection remains a challenge at CTC, these lesions tend to follow a more indolent path, most often allowing time for benign detection, the group wrote.
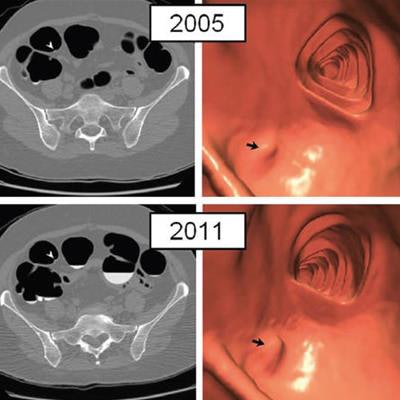
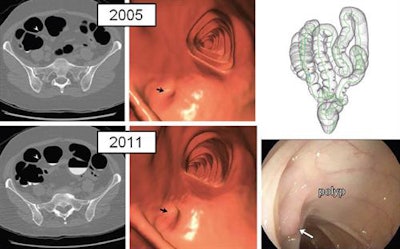 Diminutive polyp at initial CTC screening grew to small size at follow-up screening six years later in an asymptomatic woman (61 years old at initial screening). Top: 2D (left) and 3D (middle) images from initial 2005 screening show diminutive lesion (arrowhead for 2D, arrow for 3D) smaller than 5 mm in the proximal transverse colon. Bottom: 2D (left) and 3D (middle) images from repeat CTC in 2011 show that the sessile polyp has grown in the intervening six years, now measuring 7 mm. Polyp was confirmed (arrow) and removed at same-day colonoscopy (right) and proved to be a tubular adenoma at pathologic evaluation. Images republished with permission of RSNA from Radiology, August 22, 2016.
Diminutive polyp at initial CTC screening grew to small size at follow-up screening six years later in an asymptomatic woman (61 years old at initial screening). Top: 2D (left) and 3D (middle) images from initial 2005 screening show diminutive lesion (arrowhead for 2D, arrow for 3D) smaller than 5 mm in the proximal transverse colon. Bottom: 2D (left) and 3D (middle) images from repeat CTC in 2011 show that the sessile polyp has grown in the intervening six years, now measuring 7 mm. Polyp was confirmed (arrow) and removed at same-day colonoscopy (right) and proved to be a tubular adenoma at pathologic evaluation. Images republished with permission of RSNA from Radiology, August 22, 2016.Longer follow-up intervals
The fact that positivity rates for large polyps were lower at repeat screening than initial screening bodes well for stretching out follow-up intervals in the future.
"It will go even lower now that we are detecting more flat lesions on the initial screening round," Pickhardt told AuntMinnie.com. "If it drops considerably lower, we could eventually push the lower threshold of the five- to 10-year interval to perhaps seven or eight years."
More advanced right-sided lesions (including many flat, serrated lesions) may have been detected at follow-up CTC compared to the initial round due to radiologists' increasing familiarity with the lesions.
"Our results suggest that we are now much better at identifying flat right-sided lesions, many of which are serrated at histology," Pickhardt said. "However, we are also providing more evidence that these tend to be very slowly progressing, nonaggressive lesions given the relative lack of change over time."
Ignoring diminutive lesions at CTC "drives the superior cost-effectiveness of CTC, without negatively impacting clinical efficacy," the group wrote.
Among the study's limitations, the necessary exclusion from routine follow-up of individuals with an initial positive finding means that the remaining cohort would tend to have a lower colorectal cancer risk profile overall, according to the authors. Also, the results from this single-center study should not be extrapolated to practices where CTC expertise or techniques may not be the same.
"These collective findings support the practice of not reporting isolated diminutive lesions at CT colonography screening and of a five- to 10-year screening interval after initial negative examination," the group concluded.



















