Patients are said to die with -- not from -- prostate cancer. In fact, more than 90% of prostate cancer patients end up dying from something else. A new study in Radiology explored how long those patients might expect to live, using data enriched by routine CT scans that prostate cancer patients undergo before treatment.
Researchers from the University of Alabama at Birmingham looked at body composition measures in prostate cancer survivors using CT scans that patients routinely undergo. They found that CT-based measurements of bone density and muscle mass correlated strongly with survival in more than 600 prostate cancer patients (Radiology, September 5, 2016).
The large number of prostate cancer patients who die of other causes gives rise to the "fundamental question of how we can figure out a patient's risk of dying from something besides prostate cancer," said lead author Dr. Andrew McDonald in an interview with AuntMinnie.com. "The clinical history only gives you part of the information, so we looked around to see what we could do better with the information we have without a lot of additional testing."
 Dr. Andrew McDonald from the University of Alabama at Birmingham.
Dr. Andrew McDonald from the University of Alabama at Birmingham.Unique data points
CT scans of prostate cancers can provide two unique data points: bone mineral density (BMD) and muscle mass, both of which have been independently correlated with survival in previous studies. The current study aimed to determine if CT measurements of BMD and muscle mass could improve the prediction of noncancer death in men with localized prostate cancer.
"My hypothesis is that bone mineral density and muscle mass are general measures of health not picked up by other measures of health that doctors get as part of a clinical evaluation," McDonald said.
The group started with the Charlson comorbidity index (CCI), a tool for predicting the 10-year mortality risk of individuals using a basket of comorbidities, ranging from myocardial infarction history to dementia. The idea was to enhance the predictive power of CCI's mortality estimation by using CT data from prostate cancer patients, he said.
For men undergoing external-beam radiation therapy, pelvic CT is performed as part of treatment planning. CT is used to delineate target volumes and assess tissue attenuation to perform accurate dose calculations.
Several reports have confirmed that bone mineral density and total body muscle mass can be estimated accurately from abdominal and pelvic images. Meanwhile, osteopenia and sarcopenia have been associated with an increased risk of noncancer death in several different populations.
"On a pelvic CT scan, if you look at one slice at a certain level, you can really get a good idea of what that patient's overall body composition looks like -- that's an accurate approach," McDonald said. "What we did is take all patients treated for prostate cancer over a 12-year span, and we calculated values for every single one."
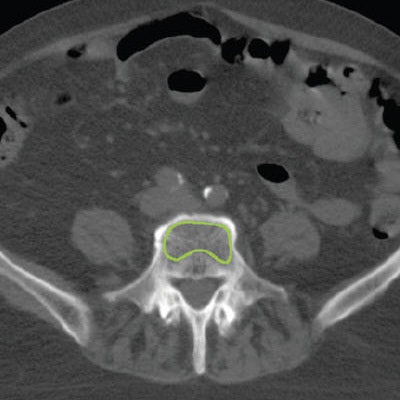
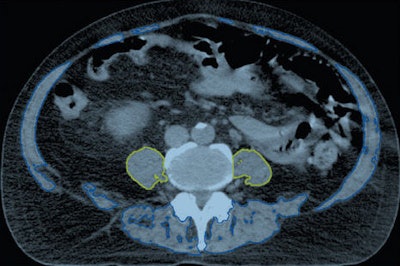 Axial CT images obtained in a 71-year-old man. Above, the bilateral psoas muscles (yellow) and total muscle area (blue and yellow) are delineated. Below, the vertebral body trabecular bone (green) is delineated. Images republished with permission from RSNA.
Axial CT images obtained in a 71-year-old man. Above, the bilateral psoas muscles (yellow) and total muscle area (blue and yellow) are delineated. Below, the vertebral body trabecular bone (green) is delineated. Images republished with permission from RSNA.Using CT performed for prostate cancer treatment planning, the researchers estimated bone mineral density at the mid-L5 level, specifically the mean CT attenuation in Hounsfield units of the trabecular bone of the L5 vertebral body, to generate a value they called L5HU. The second value, height-normalized psoas cross-sectional area, was called PsoasL4-5. The CT images were analyzed using Eclipse software (Varian Medical Systems).
The study included 653 men who received radiation therapy for localized prostate cancer between 2001 and 2012 and had their height, weight, and medical history documented. All subjects underwent CT that included the L4-5 vertebral interspace.
The researchers then generated a prognostic index for predicting noncancer death that included the two CT-generated values, age-adjusted CCI, and race, and compared it with just CCI adjusted for age.
CT-enhanced mortality prediction
The prognostic index with the CT information was superior to age-adjusted CCI, with a higher Harrell c-statistic value of 0.747 for predicting noncancer death versus 0.718 for age-adjusted CCI alone.
The group measured muscle mass (PsoasL4-5) using 7.5 cm2/m2 as the cutoff point for sarcopenia, or age-related muscle mass, with values below 7.5 cm2/m2 indicating the presence of sarcopenia. For bone mineral density, they used a threshold of 105 HU, with patients below that level at high risk of osteoporosis.
"We found that when you do account for other medical problems and you look at death as an outcome, the muscle and bone density predict death independently of each other," McDonald said.
| Independent factors predicting noncancer death | ||
| Parameter | Hazard ratio for noncancer death | p-value |
| Age-adjusted CCI | 1.36 | < 0.001 |
| PsoasL4-5 (muscle mass) | 0.003 | |
| < 7.5 cm2/m2 | 1.95 | |
| ≥ 7.5 cm2/m2 | Reference group for analysis | |
| L5HU (bone mineral density) | < 0.001 | |
| < 105 HU | 2.88 | |
| 105-150 HU | 1.42 | |
| > 150 HU | Reference group for analysis | |
| Race | 0.019 | |
| African-American | 1.68 | |
| Other | 1.77 | |
| White | Reference group for analysis | |
In short, the researchers found that patients with signs of sarcopenia had a hazard ratio of 1.95 for noncancer death, compared with those who had muscle mass levels above the 7.5 cm2/m2 cutoff. With respect to bone mineral density, those with lower BMD, measured at less than 105 HU, had a 2.88 hazard ratio, much higher than the 1.42 hazard ratio for those with a BMD between 105 HU and 150 HU.
What's more, the CT-generated measurements of bone density and muscle mass were better at predicting noncancer death than the age-adjusted CCI figure, which had a hazard ratio of 1.36.
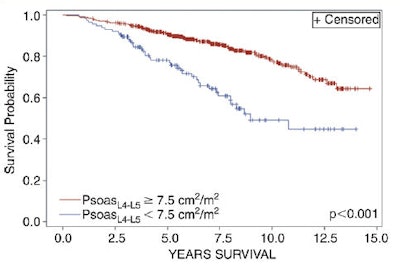 Kaplan-Meier estimates of noncancer death survival, stratified according to PsoasL4-5 (above) and L5HU (below). Images republished with permission from RSNA.
Kaplan-Meier estimates of noncancer death survival, stratified according to PsoasL4-5 (above) and L5HU (below). Images republished with permission from RSNA.The use of androgen deprivation therapy (ADT) and a patient's National Comprehensive Cancer Network (NCCN) risk group were not significant independent predictors of noncancer death. Previous studies have shown improvement in survival with ADT in some groups of prostate cancer patients. However, ADT has the drawback of decreasing bone and muscle mass, and whether ADT increases the risk of noncancer death is controversial, the group wrote.
"We need to study whether the benefit of androgen deprivation outweighs the detriment from the loss of bone from ADT," McDonald said. If he had to guess, he would say it's probably a net benefit in some patients but not others, he added.
Reducing future noise
For future research, having a study model such as this one that cuts out some of the noise of conventional mortality assessments will be crucial, McDonald said.
"If you're studying a disease where the disease only accounts for a small percentage of patients dying of the disease, you'd better design your paper correctly to balance out other causes of death," he said. "Say you have a new prostate cancer drug that works better than the other prostate cancer drugs, but with prostate cancer so few die that it adds a lot of noise to your study statistics. Taking these things into account ahead of time can balance the study in terms of patients' risk of dying of something else."
The other big take-home message from this study is that the results were obtained with existing patient data, McDonald said, and the measurements were simple to perform with commercially available software.
"There were no additional scans or additional studies, and it didn't cost another cent," he said. "The doctor really only has to spend a minute to measure these things, so it's free and relatively simple to do. And you get a good bit of information that helps you take care of patients."