CT is a reliable modality for diagnosing immune-related colitis, replacing invasive colonoscopy with high diagnostic accuracy and a safer profile, according to research published April 3 in Cancer Immunology Research.
A group from Dana-Farber Cancer Institute in Boston retrospectively analyzed patients with advanced melanoma who were being treated with the monoclonal antibody agent ipilimumab and developed gastrointestinal symptoms. Among 303 patients who received both CT and colonoscopy, CT was highly predictive of the need for steroids to resolve symptoms, with a positive predictive value of 92%, although it was less reliable for ruling out disease (Cancer Immunol Research, April 3, 2017).
"A CT scan is a useful tool to make a diagnosis of immune-related colitis that has been treated with treated with ... ipilimumab," said co-author Dr. Patrick Ott, PhD, a medical oncologist at Dana-Farber, in an interview with AuntMinnie.com. "It's basically useful to rule it in if there's a suspicion of disease, and if a CT scan has characteristic features of colitis, it has a good positive predictive value for making a diagnosis."
Life-threatening condition
Colitis can be life-threatening for patients treated with immune checkpoint blockade antibodies such as ipilimumab, which inhibits the programmed cell death protein 1 (PD1) mechanism in T lymphocytes, allowing them to destroy cancer cells. Patients treated with these antibodies can develop gastrointestinal symptoms, especially diarrhea, at any time during or after treatment. About one-third of patients develop mild symptoms, while 5% to 8% experience moderate to severe symptoms that can become serious, according to the authors.
"Differentiating between patients with mild symptoms and those who will progress to severe and life-threatening colitis is difficult, especially because presentation can be subtle and easily confused with an infectious etiology," they wrote. "Given the life-threatening nature of ipilimumab-induced colitis and the favorable response to steroids if started early, urgent and accurate diagnosis is essential."
Colonoscopy with biopsy of the colonic mucosa is the only validated tool to confirm immune-related colitis, but physicians are trying less-invasive techniques as a proxy for colonoscopy, which can cause rare but potentially serious complications such as intestinal perforation. Patients with inflamed colonic tissues are also at increased risk of complications, so noninvasive techniques would reduce exposure to the potential complications, the authors noted.
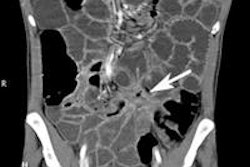
Abdominal CT is being explored as a first-line diagnostic modality that is faster, less invasive, and less risky than colonoscopy and biopsy. Imaging hasn't been previously correlated to colonoscopy and biopsy of colonic mucosa to establish a diagnosis of immune-related colitis; however, previous PET/CT studies support CT correlation with colonoscopic findings, Ott and colleagues wrote.
Comparing CT to colonoscopy, treatment
The researchers designed a study that assessed 303 metastatic melanoma patients who had received at least one dose of ipilimumab between 2008 and 2015. Patients who had at least one episode of diarrhea during ipilimumab treatment were considered for the study. Major goals were to evaluate the sensitivity, specificity, positive and negative predictive values, and positive and negative likelihood ratios of the CT scans compared with the gold standard of colonoscopy with biopsy, according to the authors.
In all, 99 (33%) of the 303 patients developed diarrhea during therapy, and 46 (15%) received corticosteroids for colitis. Among the patients with diarrhea, 48 (48%) underwent colonoscopy and 46 (46%) underwent both CT and colonoscopy.
The researchers analyzed the CT scan data in two groups. The biopsy group validated CT findings with colonoscopy and biopsy results. The steroid treatment group validated CT findings with the need for patients to receive steroid treatment for resolution of ipilimumab-induced colitis symptoms.
First, the researchers correlated bowel wall thickening, air/fluid levels, and mesenteric stranding with the histological results of colonic mucosal biopsies, which are the most definitive test for the diagnosis of colitis. Second, they correlated the CT findings with the effective use of corticosteroids in the group of 43 patients who needed steroids to resolve their gastrointestinal symptoms.
CT's high positive predictive value
In the 34 patients (34%) who had both CT and biopsy, CT was highly predictive of colitis on biopsy, with a positive predictive value of 96%. An absence of CT findings was predictive of a negative biopsy (with a negative likelihood ratio of 0.2). In addition, CT was highly predictive of the need for steroids to resolve the symptoms.
Advanced age, greater number of doses of ipilimumab, and shorter intervals between doses were associated with immune-related colitis in the 99 patients who had diarrhea and other gastrointestinal symptoms after treatment.
| Sensitivity and specificity of CT scans | ||
| CT + biopsy | CT + corticosteroid | |
| No. of patients | 34 | 47 |
| Sensitivity | 85.2% | 76.7% |
| Specificity | 75.0% | 88.2% |
| Positive predictive value (PPV) | 95.8% | 72.0% |
| Negative predictive value (NPV) | 42.9% | 68.2% |
The high PPV and relatively low NPV showed that CT was better for ruling in colitis than ruling it out, Ott said.
"If you see it and it's consistent with clinical systems, it basically really supports the diagnosis, but if CT is negative and the scans do not show anything, there could be other etiologies," he said.
If CT is negative and there is still a concern, doctors should probably treat the patient and consider colonoscopy, according to Ott.
"Patients who had immune-related colitis were older compared to patients who just had gastrointestinal symptoms but not colitis -- and they received a higher number of doses and had a shorter interval between the doses," he said.
Patients with immune-related colitis also needed more time to resolve symptoms compared to patients with gastrointestinal symptoms only. Fourteen patients needed infliximab to resolve symptoms, and colitis recurred in five patients after treatment, the authors noted. None of the colitis patients had a concurrent infection with pathogenic microbes. Bowel perforation occurred in five (1.7%) of the 303 patients treated with the drug. These patients were significantly older (mean age, 72 years) than patients without perforation (mean age, 64 years) (p < 0.012).
Not the last word
The study is not necessarily definitive, and a prospective study could be done, Ott said.
However, "it definitely provides support that one has the right diagnosis ... and we feel the data can be extrapolated more generally to immune-related colitis after checkpoint inhibitors," he said. "We are pretty confident that CT could also be used for a patient who doesn't have melanoma but has colitis from a PD1 inhibitor, which is much more prevalent now for the treatment of non-small cell lung cancer, head and neck cancer, bladder cancer, Hodgkin's lymphoma -- basically an increasing number of indications for these PD1 inhibitors that can also have colitis as a side effect."
CT is also worthy of further study for these related conditions because it is cheaper, safer, and more widely available than colonoscopy, Ott added.