CHICAGO - What if there were a low-risk, cost-effective way to validate the numerous fractional flow reserve CT (FFR-CT) technologies in development? Patient-specific 3D-printed coronary models may be the answer, according to a study presented on Monday at RSNA 2017.
Using coronary CT angiography (CCTA) scans of patients, researchers from the University at Buffalo created individually tailored 3D-printed heart models to compare the blood flow measurements of FFR-CT with those of invasive coronary catheterization. The 3D-printed models accurately replicated the anatomy and mechanical properties of the coronary arteries and allowed for testing of FFR-CT.
"3D printing offers us a unique tool for benchtop validation of diagnostic software," presenter Lauren Shepard told attendees. "Not only can this benchtop system be used for the validation and optimization of CT-derived FFR technologies, but it can also be applied to other vascular diagnostic software."
3D printing and FFR-CT
The standard method for diagnosing coronary artery disease is invasive coronary catheterization (to determine the degree of stenosis) along with fractional flow reserve (to determine the dynamics of blood flow). Though it offers the advantage of indicating appropriate treatment upon diagnosis, this invasive procedure is relatively expensive and runs the risk of inducing ischemia.
In recent years, researchers have been developing and testing several noninvasive CT-derived FFR techniques, but clinical studies for testing these software-based diagnostic tools are challenging, which emphasizes the need for benchtop experimentation methods.
To satisfy this demand, Shepard and colleagues proposed using 3D printing to provide a means of validating FFR-CT methods at a considerably lower cost and risk. First, they performed CCTA (Aquilion One, Toshiba Medical) on five patients and imported the scans into a 3D workstation (Vitrea, Vital Images), which they used to segment the coronary lumen and smooth its geometry. They then used these modified scans to create multimaterial coronary models with hollow lumens in a 3D printer (Connex3, Stratasys).
"3D printing provides a unique solution for benchtop experimentation," Shepard said.
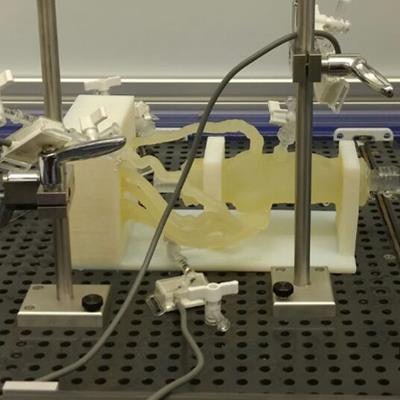
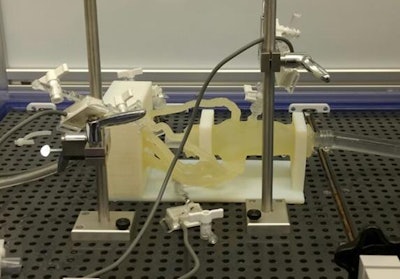 3D-printed coronary model connected to a programmable pump with pressure sensors. Image courtesy of Ciprian Ionita, PhD, from the University at Buffalo.
3D-printed coronary model connected to a programmable pump with pressure sensors. Image courtesy of Ciprian Ionita, PhD, from the University at Buffalo.The 3D-printed phantoms accurately replicated the anatomy and mechanical properties of the arterial wall, including the elasticity of vasculature, Shepard said. And when combined with a programmable flow pump and flow meters, they allowed for rapid measurement of coronary physiology and flow.
The researchers prepped the 3D-printed models for "benchtop" FFR by adding support dressing, which included distal controls to regulate incoming and outgoing flow, a flow damper to mimic aorta compliance, and a mechanical clamp to mimic resistance from the capillary bed. As a final step, they embedded the models with pressure sensors.
For the blood flow analysis, the researchers applied an algorithm using multiphase acquisition and fluid structure analysis to simulate blood flow conditions and estimate FFR. They compared the resulting measurements of FFR-CT, benchtop FFR, and catheter-based invasive FFR of the same patients.
Optimizing FFR-CT
Among the five patients examined, only one had a significant stenosis, i.e., an FFR less than 0.8. The average FFR as determined by invasive methods was 0.84. Benchtop FFR measurements using the 3D-printed models were all within 13% of invasive FFR values, with an average difference of 7%. The difference between mean benchtop FFR and FFR-CT measurements was slightly higher, at 8%.
| Comparison of FFR measurements collected by different methods | |||
| Invasive FFR | FFR-CT | Benchtop FFR | |
| Average value among 5 patients | 0.87 | 0.84 | 0.84 |
FFR measurements obtained using the 3D-printed models correlated extremely well with both invasive FFR (r = 0.9) and FFR-CT (r = 0.86).
Unlike with standard clinical methods, the benchtop 3D-printed models allowed the investigators to define a large number of blood flow conditions to validate FFR methods, according to Shepard. They also allowed the early detection of conceptual errors and a greater understanding of the software design and the limitations of its performance.
"Our preliminary results show the success of using 3D printing for FFR measurements," Shepard said. "This is an initial study, but we are expanding it to 50 patients in total."
Developed from clinical CT angiography data, the 3D-printed model offers a robust benchtop solution to test CT-FFR accurately from a geometrical, mechanical, and imaging point of view, she continued.
"Typically, patients with cardiovascular disease would undergo an angiographic study as well as a coronary CT angiography study, and those results would be compared," Shepard said. "We now incorporate a third branch -- using 3D-printed phantoms for coronary CT angiography diagnostic tools."
Industry, academia, and government researchers can use these highly customizable tools, she said.
"With continued testing of our benchtop system, we can look back at this clinical trial design and take the angiographic study, that is our standard comparison, and replace it with 3D-printed patient-specific phantoms," she said.




















