Rates of autopsy are declining, for a variety of cultural and economic reasons. But autopsy still offers valuable information about an individual's cause of death. Could an imaging-based approach replace traditional autopsy? Dutch researchers investigated this question in a study published September 25 in Radiology.
The article was the result of five years of research by the radiology and pathology departments of Erasmus University Medical Center in Rotterdam. Between 2012 and 2014 the group examined 99 deceased patients in a prospective study that compared a minimally invasive autopsy technique that combined postmortem MRI, CT, and CT-guided biopsy with traditional autopsy.

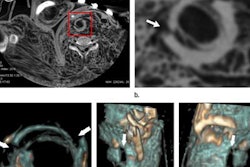
"This is the first time that a study in a clinical, rather than forensic setting, has proved that besides being equal to traditional autopsy, [minimally invasive autopsy] has additional strengths -- with imaging techniques revealing pathologies missed by traditional methods and showing doctors precisely where -- under CT-guidance -- to target tissue to obtain samples," said Dr. Annick Weustink, PhD, the study's lead radiologist and subspecialist in postmortem, cardiovascular, and musculoskeletal imaging.
"Importantly, the study also showed that while autopsy numbers are dwindling, clinicians often are not aware of cause of death. The postmortem report can serve as important feedback to improve healthcare quality and potentially other living patients' outcomes," she added.
Limited numbers
Two radiologists independently read images from 99 adult patients who died in the hospital and were included in the study, with relatively good interobserver agreement. One pathologist was responsible for histological examination of the biopsies taken during minimally invasive autopsy, with assistance from expert pathologists in their fields for consensus. Conventional autopsies took place in a routine setting by an on-call resident pathologist under supervision.
 A virtual autopsy is performed at Erasmus University Medical Center.
A virtual autopsy is performed at Erasmus University Medical Center.The primary outcome measure was performance of minimally invasive autopsy and conventional autopsy in establishing immediate cause of death, as compared with consensus immediate cause of death. The group also compared the diagnostic yield of the minimally invasive technique with conventional autopsy for all, major, and grouped major diagnoses; frequency of clinically unsuspected findings; and percentage of answered clinical questions.
Striking results
The two methods showed comparable performance in determining immediate cause of death, with agreement in 91 of 99 (92%) of cases. Minimally invasive autopsy found the consensus cause of death in 96 of 99 cases, with the technique missing one case of myocardial infarction, one case of ischemic colitis, and one case of bowel ischemia, whereas conventional autopsy found the consensus cause of death in 94 of 99 cases, misdiagnosing five cases. There was no statistically significant difference between the rates.
The minimally invasive technique made a higher total number of diagnoses than traditional autopsy, establishing 259 (90%) grouped major diagnoses related to consensus cause of death, compared with 224 (78%) of 288 for conventional autopsy.
| Causes of death correctly identified by both minimally invasive and traditional autopsy | |
| Main pathology in concordant immediate cause of death n = 91 cases | n (%) |
| Pulmonary pathology | 43 (47%) |
| Cardiac pathology | 30 (33%) |
| Sepsis/multiple organ failure/shock | 20 (22%) |
| Cerebral pathology | 10 (11%) |
| Intestinal pathology | 8 (9%) |
| Metastatic disease | 8 (9%) |
| Vascular pathology | 7 (8%) |
| Hemorrhage | 6 (7%) |
| Thromboembolic pathology | 6 (7%) |
| Hematologic disease | 5 (5%) |
| Infectious disease | 4 (4%) |
| Liver pathology | 2 (2%) |
| Urological pathology | 2 (2%) |
| Intoxication | 2 (2 %) |
| Graft-versus-host disease | 1 (1%) |
| Organ rejection | 1 (1%) |
| Storage disease (aceruloplasminemia) | 1 (1%) |
Clinician misdiagnoses
Both minimally invasive and traditional autopsy revealed that at clinical examination, doctors did not suspect the cause of death in 17 (17%) of the 99 cadavers, and did not establish 124 (43%) of the 288 grouped major diagnoses.
Specifically, in 65 (66%) of 99 cadavers, the clinically presumed cause of death was the same as the consensus cause of death, also diagnosed by minimally invasive and/or conventional autopsy. In a further 17 (17%) cadavers, reporting doctors only mentioned the consensus cause of death in the clinical differential diagnosis and not at all in the remaining 17 (17%). In the latter cases, acute pneumonia was the clinically most often missed immediate cause of death (five cases), followed by acute myocardial infarction (two cases).
Future strides
Weustink hopes the new study will generate more awareness of the potential of postmortem imaging in a clinical rather than forensic setting, and also leverage specific training for radiologists hoping to be involved in this type of innovative work.
 Dr. Annick Weustink, PhD, from Rotterdam.
Dr. Annick Weustink, PhD, from Rotterdam.In a next step, the group will soon publish the cost-related findings of both methods, in particular how costs for minimally invasive biopsy can be reduced. While the traditional procedure can be lengthy, it also takes time to perform the imaging exams and biopsies for the minimally invasive technique.
For now there are no clear cost-related answers, according to Weustink. Time taken for imaging exams and biopsies mean that minimally invasive autopsy is not a quick fix alternative to the lengthy traditional procedure, said Dr. Wolter Oosterhuis, PhD, professor emeritus of pathology at Erasmus MC.
The study comes as rates for traditional autopsy are declining everywhere, according to Oosterhuis. At Erasmus, the rate is at 10%, slightly above the national level of around 7%. Rotterdam's substantial non-Western population often declines autopsy for deceased relatives due to cultural reasons.
"This situation prompted us to look at a new, less-invasive autopsy method that is more acceptable to next-of-kin, but that yields answers to clinical questions. Feedback from the families who gave consent for both methods suggested that many would have been happier to have their relatives autopsied using only [minimally invasive autopsy]," he said.
 Dr. Wolter Oosterhuis from Rotterdam.
Dr. Wolter Oosterhuis from Rotterdam.The advantages of the minimally invasive method included perfect depiction of pathologies such as pneumonia, sometimes overlooked in traditional autopsy due to the thickness of organ slices. In addition, MRI appeared highly sensitive for guiding tissue sampling in the diagnosis of acute myocardial infarction. However, the minimally invasive approach had trouble identifying bowel ischemia, because it is difficult to spot early necrosis in the bowel wall or obtain samples when it can be seen.
Oosterhuis pointed to the important role that autopsy of any kind plays in the quality assurance of patient care.
"It is clear that people are dying of causes that clinicians aren't aware of. We don't know if a premortem diagnosis of acute pneumonia could have saved the patient's life, but it might save the next patient if the clinician is made aware of it in the postmortem report," he said.
Autopsies still have an important function when examining the cause of death of hospitalized patients, and the unanswered question now is what form they will take and how acceptable the techniques are to the individual's family, he noted.