Current guidelines used to determine the effect of cancer treatment on metastatic tumors often yield inconsistent results, say researchers from Germany, who uncovered notable differences in tumor selection on CT among radiologists. Their findings were published online November 6 in Radiology.
The group, led by first author Dr. Christiane Kuhl from University Hospital Aachen, examined nearly 1,000 baseline and follow-up CT scans of patients who received systemic treatment for metastatic cancer. The researchers referred to the standardized Response Evaluation Criteria in Solid Tumors (RECIST) to evaluate cancer progression and treatment efficacy on the patients' CT scans.
Prior research has suggested that the RECIST guidelines are likely not sensitive enough for tumor assessment, and several groups have questioned the consistency of results acquired following these criteria.
In light of these issues, Kuhl and colleagues evaluated the quality of assessments made using RECIST for 316 patients.
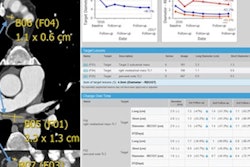
At least three radiologists among a total of five independently reviewed the metastatic tumors on the patients' CT scans based on the RECIST guidelines. Using computer software (Mint Lesion v2.6.4, Mint Medical), the radiologists selected and measured five tumors, including the largest measurable tumor, that they believed best represented the metastatic cancer. They subsequently measured and classified these target lesions on each of the patients' follow-up CT scans to determine any changes in size and response to treatment.
For all patients, the readers ended up selecting the same group of representative tumors only 40.5% of the time and different tumors 59.5% of the time, despite using the same RECIST-based selection criteria.
When the collection of representative tumors for a patient chosen by the radiologists was concordant, or the same, the resulting agreement in tumor classification was very high. In contrast, discordant tumor selection was associated with widely inconsistent assessments of tumor progression.
| Concordant vs. discordant tumor selection on CT for tumor progression assessment | ||
| Concordant tumor selection | Discordant tumor selection | |
| Reader agreement on tumor progression | 97.7% of cases | 55.3% of cases |
"Target lesions selected and measured in strict adherence to RECIST 1.1 guidelines are not necessarily representative of the overall tumor load," the authors wrote.
The variability in tumor progression assessment among the radiologists was large enough to lead to different treatment recommendations for a number of patients, they noted.
What are potential solutions for improving the consistency of tumor selection as well as the assessment of tumor progression on CT?
Kuhl and colleagues suggested that more refined criteria on how to select target lesions would be a good place to start.
Another possible long-term solution may be to develop an artificial intelligence algorithm to ensure uniform lesion selection and more precise measurements, wrote Dr. Jacob Sosna of Hadassah Medical Center in Israel in an accompanying editorial.
"It is time for a deeper understanding of the follow-up methods used, along with their strengths and weaknesses, to ensure reliable response assessment for improved patient care," he wrote.