Researchers from the U.S. have linked vaping to the development of severe respiratory illnesses identified on CT scans, according to a report published online September 6 in the New England Journal of Medicine. The findings indicate that marketing claims attesting to the safety of vaping with electronic cigarettes (e-cigarettes) may have been misleading.
In their study, the group of researchers identified a cluster of recent cases indicating a potentially causative relationship between the use of e-cigarettes and severe pulmonary disease in otherwise young, healthy individuals.
"Since no single product or substance has been associated with the illness, persons should consider not using e-cigarettes while this investigation is ongoing. ... Irrespective of these findings, e-cigarettes should never be used by youths, young adults, pregnant women, and adults who do not currently use tobacco products," wrote lead author Dr. Jennifer Layden, PhD, chief medical officer of the Illinois Department of Public Health, and colleagues (NEJM, September 6, 2019).
Vaping triggers lung disease
E-cigarettes span a wide range of battery-powered devices that vaporize liquid nicotine and similar substances for inhalation. Though marketed as a relatively safe alternative to smoking, e-cigarettes are known to contain substances -- including volatile organic compounds, heavy metals, and ultrafine particles -- that have adverse health effects.
As recently as July 2019, a cluster of medical reports has emerged in Wisconsin and Illinois indicating a potential association between various lung diseases and the use of e-cigarettes, commonly referred to as vaping. These reports subsequently prompted the Wisconsin Department of Health Services and the Illinois Department of Public Health, with assistance from the U.S. Centers for Disease Control and Prevention (CDC), to launch a joint public health investigation.
In their preliminary report, Layden and colleagues evaluated 53 patients categorized as having a vaping-related illness, 93% of whom were hospitalized and one of whom died. The cases only included previously healthy individuals who reported using e-cigarettes and related products within 90 days before the onset of symptoms not attributed to other causes and whose chest x-ray or CT scans displayed opaque substances (i.e., pulmonary infiltrates) in both lungs.
The patients presented with a combination of respiratory, gastrointestinal, and constitutional symptoms, the most common of which included shortness of breath (87%), nausea (70%), and vomiting (66%). All the CT scans acquired turned out to have abnormal findings.
After examining the cases, the researchers identified similar clinical features and disease progression among the patient cohort, despite being affected by a range of severe pulmonary illnesses. The clinical presentation of these patients most likely appeared to result from acute toxic lung injury, they concluded.
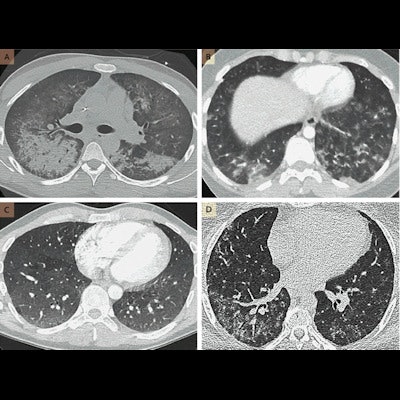
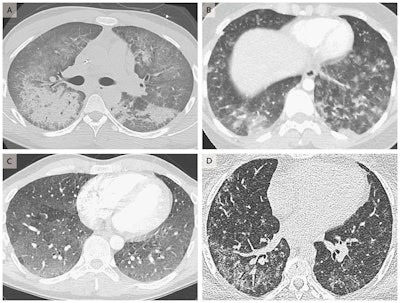 Chest CT scans showing diffuse alveolar damage in the lungs of a 20-year-old man (A), acute eosinophilic pneumonia in a 19-year-old woman (B), hypersensitivity pneumonitis in a 35-year-old man (C), and giant-cell interstitial pneumonia in a 49-year-old-woman (D). The symptoms of these patients improved after vaping cessation. Image courtesy of The New England Journal of Medicine ©2019.
Chest CT scans showing diffuse alveolar damage in the lungs of a 20-year-old man (A), acute eosinophilic pneumonia in a 19-year-old woman (B), hypersensitivity pneumonitis in a 35-year-old man (C), and giant-cell interstitial pneumonia in a 49-year-old-woman (D). The symptoms of these patients improved after vaping cessation. Image courtesy of The New England Journal of Medicine ©2019.The majority (84%) of the patients claimed to have used e-cigarettes to inhale tetrahydrocannabinol (THC), though the devices delivered a wide variety of other products, including nicotine and cannabidiol (CBD). Approximately 80% of those who vaped and fell ill also said that they used both nicotine and either THC or CBD products.
The mixing of these different ingredients, along with the thermal decomposition of other known contaminants in e-cigarette fluids, could have sparked the production of new toxic agents, according to the authors. And subsequently, these agents may have triggered the pulmonary illnesses.
Regarding their medical care, all but two patients recovered after receiving various forms of treatment, including vaping cessation, intubation, oxygenation, and glucocorticoid therapy. Thus far, all patients who received systemic glucocorticoids have shown improvement, although the current understanding of appropriate treatment strategies is too limited to offer clinical recommendations, the authors noted.
Clear epidemic
Further corroborating these findings, two additional reports published September 6 in the NEJM attested to the rising occurrence of vaping-induced respiratory distress in other regions of the U.S.
First, Dr. Sean Maddock and colleagues from the University of Utah Health identified a cluster of six cases in the state that paralleled the findings reported by Layden and colleagues. The most severe case involved a previously healthy 21-year-old man whose CT scans revealed diffuse consolidative opacities and was found to have acute respiratory distress syndrome. The symptoms appeared some time after he began to daily vape nicotine and THC, and the condition improved after several days of oxygen treatment and vaping cessation.
The second study, led by Dr. Travis Henry from the University of California, San Francisco, reported 19 cases in California and Wisconsin that met the criteria for vaping-associated lung injury. They identified several imaging patterns that appeared to correlate with pathology caused by vaping, including signs on CT scans indicating acute eosinophilic pneumonia, diffuse alveolar damage, organizing pneumonia, and lipoid pneumonia.
In late August 2019, the CDC tallied 450 suspected cases of vaping-related illness in the U.S., three of which have resulted in death. The CDC is now coordinating a public health response in several states throughout the country. Contributing to that end, the U.S. Food and Drug Administration (FDA) has already begun analyzing more than 120 vaping product samples that were used by these patients.
"I want to stress that more information is needed to determine which specific products or substances are involved ... to better understand if a true relationship exists between any specific product or substance and the illnesses we are observing in patients," noted Dr. Dana Meaney-Delman of the CDC in a statement.
"Although more investigation is needed to determine the vaping agent or agents responsible, there is clearly an epidemic that begs for an urgent response," Dr. David Christiani, of the Harvard T.H. Chan School of Public Health, wrote in an accompanying editorial.
As researchers continue seeking out the exact compound or compounds that cause these health concerns, "efforts should be made to increase public awareness of the harmful effect of vaping, and physicians should discourage their patients from vaping," he concluded.