CHICAGO -- The diagnosis of electronic cigarette (e-cigarette) or vaping-associated lung injury (EVALI) on imaging exams continues to evolve as reports of new cases emerge daily. A panel of experts on the subject shared their insights into the epidemic in a special interest session at RSNA 2019.
Anecdotal cases of EVALI have been identified in various hospitals throughout the U.S. as far back as 2014, but it was not until examining the flurry of reports released earlier this year that scientists and clinicians have been able to piece together a somewhat fluid set of criteria for diagnosing the condition.
Still, EVALI diagnosis remains relatively uncertain in more cases than not. For instance, a 48-year-old woman recently assessed by Dr. Travis Henry and colleagues at the University of California, San Francisco seemed to meet all of the criteria for an EVALI diagnosis: She had vaped e-cigarettes within the past 90 days, showed pulmonary infiltrates on an imaging exam, and had other possible causes of injury ruled out. Yet the group was unable to state conclusively that her symptoms were entirely due to vaping.
The uncertainty surrounding EVALI stems in large part from the novelty of the condition and not knowing the long-term effects of the disease, Henry told session attendees. "What is certain is that e-cigarettes aren't going away -- there's too much money involved, too much politics, and there is some potential benefit for specific populations."
What we know thus far
As of late November, roughly 2,300 cases of EVALI have been reported to the U.S. Centers for Disease Control and Prevention (CDC) from 49 states (all but Alaska); Washington, DC; Puerto Rico; and the Virgin Islands. The median age of the cohort is 24 years, 95% of the cases have required hospitalization, and nearly 50 patients have died.
Dr. Mark Schiebler from the University of Wisconsin School of Medicine and Public Health mentioned several other findings that help characterize the vaping epidemic, including the following:
- E-cigarette vaping has increased sharply among high school and middle school students in the past two to three years.
- The ratio of males to females diagnosed with EVALI is about seven to three.
- Though the exact composition of many vaping products is not disclosed, early analysis of lung fluid has indicated that THC and vitamin E acetate have a stronger association with lung injury than nicotine agents. The CDC recently disclosed that 100% of the fluid samples submitted for analysis (29 in all) turned out to contain vitamin E acetate. And quantitative MRI analysis confirmed EVALI in cases where nicotine was not inhaled.
- The size of particulate matter is directly linked to health issues. Radiologists should take note of particles smaller than 2.5 µm, as they can bypass the bronchial/mucosal safety net, penetrate the lung periphery, and diffuse into the bloodstream, Schiebler noted.
- The total number of reported cases per day peaked in September and has been on the decline since then, although clinicians are still confirming cases by the dozens.
4 main imaging patterns
For radiologists, perhaps the most important thing is keeping an eye out for lung disease patterns that could indicate EVALI, noted Dr. Seth Kligerman, division chief of cardiothoracic radiology at the University of California, San Diego (UCSD).
"Because many people are just not thinking about it," he said. "And I believe it's very beneficial to think about it because you can help these patients start getting better by getting them on steroids quickly."
After examining at least 65 EVALI cases in just the past several months, Kligerman and colleagues at UCSD recognized four patterns on chest x-ray and CT scans that appeared more often than the rest:
- Organizing pneumonia: By far the most common imaging pattern, organizing pneumonia is marked by bilateral ground-glass opacity with mild consolidation, septal thickening (including a "crazy paving" pattern), and striking subpleural and perilymphatic sparing, often in the central portions of the lung around the heart. Most EVALI predominantly affected by organizing pneumonia tend to recover quickly after steroid treatment.
Diffuse alveolar damage: Diffuse alveolar damage is similarly characterized by ground-glass opacities, perilymphatic sparing, and septal thickening, but the pattern is associated with a relatively higher mortality rate. In some instances, follow-up imaging two weeks after initial diagnosis showed subpleural blebs near regions of the lung that were being destroyed, resulting in permanent fibrosis. Many of these patients ended up dying a few weeks later, despite steroid treatment.
In addition, these patients occasionally have an accompanying pattern of acute eosinophilic pneumonia with increased fluid and capillary leak. Eosinophilic pneumonia often presents in later stages of the disease and could lead to a delay in diagnosis.
- Diffuse alveolar hemorrhage: Identifying this pattern usually requires a combination of chest imaging and bronchoalveolar lavage (BAL) in order to distinguish it from other causes of acute lung opacities such as edema or infection.
- Centrilobular nodularity: In some cases, extensive centrilobular nodules are the most conspicuous finding. The challenge lies in its long differential diagnosis, which includes hypersensitivity reactions, airway centered organization, hemorrhage, and other causes of inflammation or injury to the respiratory bronchioles.
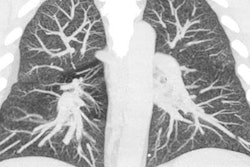
 Above: CT image of a 51-year-old woman who recently quit smoking and starting vaping nicotine one week prior to examination. Below: Radiograph of a 51-year-old woman who recently quit smoking and starting vaping nicotine one week prior to examination. All images courtesy of Dr. Seth Kligerman from the University of California, San Diego.
Above: CT image of a 51-year-old woman who recently quit smoking and starting vaping nicotine one week prior to examination. Below: Radiograph of a 51-year-old woman who recently quit smoking and starting vaping nicotine one week prior to examination. All images courtesy of Dr. Seth Kligerman from the University of California, San Diego.Questions remain
Recent pathological examination of EVALI cases has also helped refine current understanding of the disease.
At the Mayo Clinic in Phoenix, Dr. Brandon Larsen, PhD, and colleagues examined histologic sections of cryobiopsy samples and identified centrilobular nodules even at the lowest magnification. Higher magnification of the slides showed acute lung injury patterns marked by fibrin and chronic inflammatory cells, interstitial and submucosal edema, and sloughing of epithelial cells with foamy macrophages and other debris in the airway lumen, among other pathologies.
They also found that many EVALI cases showed lipid-laden macrophages in their bronchoalveolar lavage fluid. The most common pathology injury was organizing pneumonia, but EVALI was not linked to exogenous lipoid pneumonia; pneumonia is characterized by large white holes, whereas EVALI displayed a wide range of injuries in various stages of organization, according to Larsen. Collectively, there was no overarching finding that united all the cases, and the disease processes appeared to be very different on different pathology slides.
What's more, histology confirmed that the presentation of EVALI changed over time, with the first few days dominated by edema and fibrin, inflammation setting in roughly five or six days after diagnosis, and fibroplasia appearing after about seven days. This suggests that the time of biopsy after EVALI presentation could make a big difference, Larsen noted.
"This is the first time I've seen systematic destruction of the lungs like this," Kligerman said to conclude the session. "And these are just the acute injuries. We don't know about the long-term consequences of this. ... In 20 to 30 years -- or maybe in five years -- are we're going to be having an outbreak of a severe interstitial lung disease we haven't seen before? We just don't know."