
Does COVID-19 have a more devastating effect on pregnant women? Is the disease passed down to newborns after birth? What's the best management strategy for this vulnerable population? Researchers from China addressed these and similar questions in a March 18 study published in the American Journal of Roentgenology.
Prior outbreaks such as severe acute respiratory syndrome (SARS) and the swine flu have proved to be particularly dangerous during pregnancy. Reports have indicated that death rates were as high as 25% for pregnant women with SARS and that pregnant women were four times more likely to be hospitalized for the swine flu than the general population, noted the researchers, led by Dr. Dehan Liu of Huazhong University of Science and Technology.
Whether pregnant women are more susceptible to the negative effects of COVID-19 remains to be seen. In the current study, Liu and colleagues reviewed the clinical data and CT exams of 15 pregnant women diagnosed with COVID-19 pneumonia, with gestational ages ranging from 12 to 38 weeks.
All the patients tested positive for SARS-CoV-2, the virus that causes COVID-19, on reverse transcription polymerase chain reaction (RT-PCR) between January 20 and February 10. Approximately 87% presented with fever, and 60% also had a cough, though 13% showed no clinical symptoms of COVID-19.
The women received instruction on breath holding, had their lower abdomen and pelvis covered with a lead blanket, and signed an informed consent form before undergoing initial and follow-up chest CT exams.
As a whole, the CT scans predominantly displayed ground-glass opacity in the early stage of COVID-19. The CT features evolved into patches of crazy-paving patterns and consolidation as the disease progressed, with lesions showing absorption by the final stage of the disease. Disease distribution was chiefly in the lower lobes, at 96% of all cases; involvement in the upper lobes was present in 52% to 72% of cases.
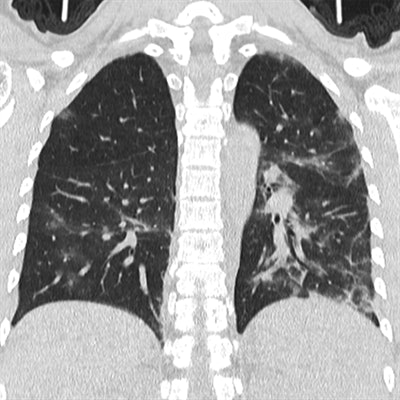 CT images of a 29-year-old pregnant woman with mild pneumonia from COVID-19. Images obtained during peak disease stage show multiple ground-glass opacities with bilateral partial consolidation (above) and during the final absorption stage six days later (below). Images courtesy of the American Journal of Roentgenology (AJR).
CT images of a 29-year-old pregnant woman with mild pneumonia from COVID-19. Images obtained during peak disease stage show multiple ground-glass opacities with bilateral partial consolidation (above) and during the final absorption stage six days later (below). Images courtesy of the American Journal of Roentgenology (AJR).The researchers additionally used a semiquantitative CT technique to estimate the extent to which abnormalities affected the lungs.
On average, the patients' CT score indicated less than 1% pulmonary involvement during the early stage of the disease. The average amount of involvement gradually increased in correlation with increasing disease progression, from roughly 25% during the progressive stage of the disease to a peak of about 26% to 49% involvement during the final absorption stage.
Furthermore, symptoms of COVID-19 disappeared in all 15 women after treatment with antibiotics during pregnancy and with antivirals after delivery. The researchers found no evidence of relapse or aggravation of pneumonia symptoms during pregnancy or after childbirth. All save one woman tested negative for SARS-CoV-2 on RT-PCR testing by the end of the study.
Among the 11 births delivered during the study, no cases of neonatal death or asphyxia occurred. None of the children showed any evidence of SARS-CoV-2 infection, and all the newborns were deemed healthy based on Apgar scores recorded at minutes 1 and 5 after birth. The births included one vaginal delivery and 10 cesarean sections.
"Pregnancy and delivery did not aggravate the severity of COVID-19 pneumonia," the authors wrote. "In addition, our results raise the question of whether antiviral therapy is necessary for pregnant women with COVID-19 pneumonia and ... should be evaluated for potential risks to the fetus considering both drug toxicity and the viral infection."




















