It's the middle of the night, only one radiologist and one CT technologist are on duty, and the emergency department calls to say 15 patients with suspected COVID-19 are heading to CT for imaging. Is your department ready?
In a letter published April 6 in the Journal of the American College of Radiology, researchers from the University of Southern California emphasized that it's critical to take proactive measures now to prepare for a "mass casualty incident" -- that is, an event like the COVID-19 pandemic that can overwhelm a hospital's resources.
This kind of scenario "illustrates the importance of involving the radiology department in the hospital's mass casualty incidence plan," wrote a team led by Dr. Lee Myers. "Conventionally, this would include terrorist attacks, bombings, mass shootings, or natural disasters. An infectious disease outbreak, however, could also quickly exhaust a hospital's resources. In the case of a viral outbreak such as the coronavirus disease 2019 ... the inciting event leads to a more protracted course of resource utilization and depletion."
Tremendous stress
Radiology plays an important role in triaging and diagnosing patients during a medical emergency, Myers and colleagues noted. But "even the most efficient radiology department will undergo tremendous stress when victims of a mass casualty flood the emergency department."
"Healthcare systems worldwide should be prepared for an unusually high volume of patients in the next few months," the authors wrote. "This will include patients with COVID-19 in addition to patients requiring emergent care for other illnesses."
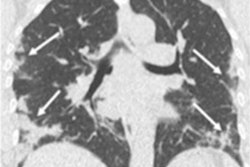
Reverse transcription polymerase chain reaction (RT-PCR) assays are considered the best way to identify COVID-19, but it can take time to get results, and a negative test doesn't necessarily exclude the disease, the team noted. CT offers a way to detect COVID-19 in patients manifesting symptoms.
"It is expected that there will be significant interest in increasing the number of imaging studies ordered for suspected cases of COVID-19 from both the emergency department and inpatient services," Myers and colleagues wrote.
The team offered a number of suggestions to help radiology departments gear up for a health emergency such as a surge in COVID-19 cases.
Get ready.
- Communicate with the hospital's emergency medicine leadership and review its mass casualty incident plan.
- Develop a protocol for cleaning x-ray machines and CT and ultrasound scanners.
- Coordinate with the hospital's environmental services on protocols for cleaning CT, MRI, and x-ray rooms.
- Maintain updated contact information for radiology, emergency medicine, and infectious disease staff. "The radiology leadership, chief technologist and the [mass casualty incident] plan liaison should communicate at least daily to evaluate the needs of emergency department and inpatient services," the group wrote.
Mobilize.
- Dedicate a CT scanner for use only with patients suspected of having COVID-19.
- Marshal more ancillary staff and CT technologists as imaging use increases. "As more infected patients arrive to the hospital, the radiology department may become overwhelmed, especially if chest CT is utilized for screening," the authors wrote.
- Use portable equipment to minimize disease transmission by reducing the number of patients being moved around the hospital.
- Assign portable x-ray units to the emergency department.
Clarify.
- Determine who will order CT exams and which patients will be deemed eligible for them.
- Establish the CT protocol: standard or low dose?
- Decide who will schedule the next patient and establish a transport process.
- Implement an after-imaging scanner cleaning protocol.
- Determine how imaging findings will be communicated. "Consider templates specific for coronavirus," Myers and colleagues suggested.
Refine.
- Adjust imaging protocols for other trauma patients and limit time-intensive studies such as gated CT angiography.
- Establish a designated area for patients suspected of COVID-19 to wait for their exam, sitting at least 6 ft apart and wearing masks to prevent transmission.
Practice.
- Run simulations to determine how much extra staff is needed and identify areas of bottleneck. Consider factors such as imaging turnaround time from order, where patients wait to be imaged, and what the waiting area capacity is.
- Provide in-service training for technologists by imaging specialty, ancillary staff, patient transporters, and radiology supervisors. Make it clear who staff should call if and when additional resources are needed.
Radiology must prepare
The radiology department must prepare for a surge in COVID-19 cases, the team concluded.
"Having a mass casualty incident plan in place for a viral outbreak will protect patients and staff and ultimately decrease virus transmission," the group wrote. "The radiology department should be ready to mobilize equipment and staff to meet the needs of our patients."