
The Fibrosis-4 (FIB-4) index and multiple CT findings can identify patients with high-risk nonalcoholic fatty liver disease (NAFLD), according to new research published on January 21 in the American Journal of Roentgenology. However, nonalcoholic steatohepatitis (NASH) remains undetectable on CT.
Dr. Meghan G. Lubner from the department of radiology at the University of Wisconsin School of Medicine and Public Health and colleagues reviewed 186 patients with biopsy-proven NAFLD who underwent CT within one year of biopsy to determine the utility of laboratory and CT metrics in identifying patients with high-risk NAFLD.
If a patient showed presence of any lobular inflammation and hepatocyte ballooning, they were classified as having NASH, while patients with NAFLD and advanced fibrosis (stage F3 or higher) were determined to have high-risk NAFLD.
The researchers found 87 patients (47%) had NASH and 112 (60%) had moderate to severe steatosis. They classified a total of 51 patients as fibrosis stage F0, 42 as F1, 23 as F2, 37 as F3, and 33 as F4. The researchers also determined 70 (38%) had advanced fibrosis (stage F3 or F4) and were considered to have high-risk NAFLD.
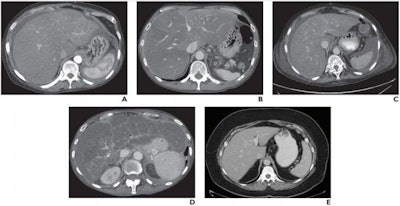 A and B, true-positive assessments in 58-year-old woman (A) and 52-year-old man (B) with high-risk NAFLD and associated NASH. CT images show hepatic enlargement, heterogeneously low-attenuation hepatic parenchyma, and surrounding ascites. Readers correctly identified NASH according to these imaging features. Readers also correctly identified fibrosis stage F3. C and D, False-positive assessments in a 73-year-old woman (C) and a 61-year-old woman (D) with high-risk NAFLD but without pathologic evidence of NASH. CT images show findings similar to A and B. Readers incorrectly identified NASH because of these imaging findings but correctly identified fibrosis stages F3 (C) and F4 (D). E, False-negative assessment in a 56-year-old woman. CT image shows liver is not enlarged, heterogeneous, or low in attenuation, and ascites is not present. Both readers interpreted the image as not showing findings indicative of NASH. However, NASH was diagnosed from surgical pathology. Image courtesy of American Roentgen Ray Society, American Journal of Roentgenology.
A and B, true-positive assessments in 58-year-old woman (A) and 52-year-old man (B) with high-risk NAFLD and associated NASH. CT images show hepatic enlargement, heterogeneously low-attenuation hepatic parenchyma, and surrounding ascites. Readers correctly identified NASH according to these imaging features. Readers also correctly identified fibrosis stage F3. C and D, False-positive assessments in a 73-year-old woman (C) and a 61-year-old woman (D) with high-risk NAFLD but without pathologic evidence of NASH. CT images show findings similar to A and B. Readers incorrectly identified NASH because of these imaging findings but correctly identified fibrosis stages F3 (C) and F4 (D). E, False-negative assessment in a 56-year-old woman. CT image shows liver is not enlarged, heterogeneous, or low in attenuation, and ascites is not present. Both readers interpreted the image as not showing findings indicative of NASH. However, NASH was diagnosed from surgical pathology. Image courtesy of American Roentgen Ray Society, American Journal of Roentgenology.In terms of the laboratory and CT metrics, a FIB-4 score showed correlation with fibrosis, and so did liver segmental volume ratio and splenic volume on CT. Lubner and her team found FIB-4 and subjective scores were complementary, and FIB-4 performed best for NASH assessment.
They concluded CT can be a tool to assess patients with NAFLD and identify those with high-risk NAFLD who are potentially most in need of intervention.




















