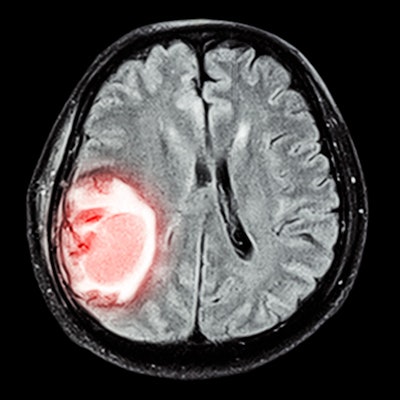
Ambulances fitted to function as mobile stroke units -- with CT, point-of-care lab testing, and thrombolysis capabilities -- improved the outcomes among patients who suffer acute ischemic stroke, according to a study published February 2 in JAMA.
The findings are good news for these patients, wrote a team led by Dr. Martin Ebinger of Charité-Universitätsmedizin Berlin.
"Mobile stroke units shorten the time to treatment, increase thrombolysis rates, and improve prehospital triage," the team wrote.
Faster is better
Thrombolytic therapy -- dispensing drugs that dissolve blood clots in the arteries or veins -- is most beneficial when it is administered as soon as possible after a stroke occurs, Ebinger's group noted. Since there are few data on the effect of mobile stroke units on patients' functional outcomes after stroke, the researchers conducted a study using emergency calls/ambulance dispatch information from Charité between February 2017 and October 2019. The study included 1,543 patients, to whom 749 were sent both the mobile stroke unit and a conventional ambulance and to whom 794 were sent a conventional ambulance only.
If an emergency call suggested stroke, both a conventional ambulance and a mobile stroke unit were dispatched if the mobile unit was available; some patients were marked eligible for a mobile stroke unit but were only sent a conventional ambulance because a mobile stroke unit was not available. The mobile stroke units included a CT scanner that allows for angiography, telemedicine connections to radiologists, and a point-of-care laboratory that can measure blood cell count, blood glucose, creatinine, and electrolytes; staff included a paramedic, a radiology technician with emergency training, and a neurologist.
Ebinger and colleagues assessed three-month functional outcomes of any patients out of the total cohort who received a final diagnosis of acute cerebral ischemia who were eligible for thrombolysis or thrombectomy at the time of the emergency call using a modified Rankin scale (range, 0 to 6, with 0 equal to no symptoms and 6 equal to death). These outcomes were compared based on the initial dispatch situation.
The investigators found that the posting of a mobile stroke unit improved patient outcomes at three-month follow-up, with those who received the mobile unit having median modified Rankin scale scores of 1 compared with 2 for those to whom a mobile unit was not sent.
The team also found the following information about patients who were dispatched a mobile stroke unit:
- 13 deaths occurred within seven days of the original call, compared with 24 deaths within seven days among patients who were not dispatched a mobile unit.
- The rate of thrombolysis was higher and the median dispatch-to-thrombolysis time was lower compared with those to whom a mobile unit was not sent out.
The study offers evidence that a "faster start of a time-dependent therapy provided in mobile stroke units is associated with better functional outcomes" in patients suffering acute strokes, Kristi Bache, PhD, of the University of Oslo in Norway, and Dr. James Grotta of Memorial Hermann Hospital-Texas Medical Center in Houston, wrote in an accompanying editorial.
"Ebinger and colleagues provide the first convincing evidence that mobile stroke units, compared with conventional ambulances transporting patients to an emergency department, treat more patients with acute ischemic stroke, treat them faster, and improve their outcomes," Bache and Grotta concluded.