More than a year into the COVID-19 pandemic, it's becoming clear that some patients experience chronic, long-term symptoms from the disease, and if the number of these "long-haulers" increases, the trend will have a significant effect on radiology, according to a poster at the virtual American Roentgen Ray Society (ARRS) meeting.
Dr. Lillian Chiu of New York Medical College in Valhalla, NY, and colleagues outlined the possible effects on radiology going forward into a "postpandemic" future, emphasizing the need for radiology departments to be prepared.
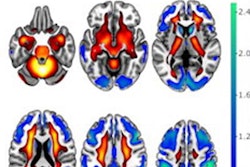
"Although we continue to know little of this disease and the short- and long-term effects, we expect there will be increased utilization of radiology imaging studies to help define complications and long-term sequela of COVID-19," the group wrote. "These may include brain and cardiac imaging studies as well as imaging follow-up for complication of lung disease."
Most patients who suffer from COVID-19 have mild to moderate symptoms and recover within two to six weeks, Chiu's team noted. But some have symptoms that recur for months after initial recovery, including fatigue, dyspnea and cough, chest or joint pain, headache or myalgia, loss of taste or smell, and sore throat -- as well as brain fog and long-term cardiac complications.
These patients have been dubbed "long-haulers," and it appears that they are more often 50 years of age or older and have chronic additional conditions like hypertension, obesity, or immunosuppressive disease. Patients struggling with chronic COVID-19 symptoms tend to require prolonged rehabilitation, and some experience mental health complications and stress, according to Chiu and colleagues.
"The effects we are seeing may only be the tip of the iceberg," they warned.
Imaging has played a key role in the diagnosis, management, and follow-up of COVID-19 patients, and this role will continue to evolve as the crisis continues, the group wrote. Over the course of the pandemic, radiologists have discovered which modalities are most effective for diagnosing and managing COVID-19.
But COVID-19 has had dramatic effect on the specialty, including a negative economic impact -- especially on outpatient imaging -- and changed work patterns (such as working from home or imaging workflow disruptions due to more rigorous equipment and room cleaning protocols).
The disease shows little sign of being vanquished for good, and radiologists must remain vigilant, especially regarding increases in caseload and referring physician consult requests, Chiu's group noted.
"As cases continue to rise around the country and the globe, the number of long-haulers may increase," the team wrote. "If imaging is part of the workup, it could potentially increase resource utilization in [the] radiology department."
Departments that plan for negative scenarios will be able to adapt and recover more easily, according to Chiu and colleagues.
"Administrators and radiology leaders may want to consider how the department would handle a sudden increase in imaging volumes and consultations," they concluded. "Preparedness should consider staffing, availability of equipment, and collaboration with other departments."