CT coronary artery calcium (CAC) scoring appears to be a useful way to help clinicians ascertain whether a patient at intermediate risk for atherosclerotic cardiovascular disease (ASCVD) would benefit from statin therapy, according to a study published July 14 in JAMA Cardiology.
It can be difficult to establish whether statin therapy would be helpful in this patient population just by assessing risk factors -- which is why CT CAC can help, wrote a team led by Dr. Jaideep Patel of Virginia Commonwealth University Medical Center in Richmond, VA.
"For cases in which additional risk stratification is required or uncertainty exists regarding the use of statin therapy, coronary artery calcium scoring may be used to further guide the clinician-patient risk discussion," the group wrote.
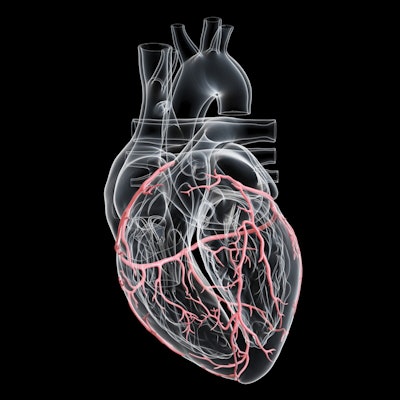
High CAC scores often indicate subclinical atherosclerosis, since coronary plaque burden is associated with events related to atherosclerotic cardiovascular disease, according to Patel and colleagues. The most current guideline from the American Heart Association and American College of Cardiology for managing blood cholesterol recommends assessing patient risk factors and using CT CAC scoring to guide use of statin therapy among people at intermediate risk of atherosclerotic CVD. But determining the need for this therapy gets complicated when a patient has risk factors for heart disease but a CAC score of 0.
Patel's group explored the association between risk factors for atherosclerotic CVD and CAC scores via a study that included data from 1,688 patients in the Multi-Ethnic Study of Atherosclerosis (MESA). MESA's baseline data were collected between July 2000 and July 2002; participants were tracked for ASCVD events through August 2015.
None of the participants had atherosclerotic CVD at baseline but all were at intermediate risk (7.5% to 20%) due to traditional risk factors such as family history of the condition, premature menopause, metabolic syndrome, chronic kidney disease, lipid and inflammatory biomarkers, or a low ankle-brachial index (which measures blockage of the arteries in the legs).
The team found that over the median follow-up of 12 years, the incidence rate of ASCVD among those participants with a CAC score of 0 was less than 7.5 events per 1,000 person years for all risk factors (except the ankle-brachial index, which had a rate of 10.4 events per 1,000 person years, the group noted).
The highest rate of atherosclerotic CVD was found in individuals who had CAC scores of 100 or more, and three or more traditional risk factors. These individuals experienced 12.7 events per 1,000 person years.
How do these results translate to clinical practice? They suggest that CT CAC scoring can help clinicians better categorize patients at intermediate risk of ASCVD, according to the team.
"The use of CAC scoring was associated with significant improvements in the reclassification and discrimination of incident ASCVD and may therefore be useful as an adjunct to risk-enhancing factors to identify individuals with intermediate risk of ASCVD who would benefit from statin therapy," the authors concluded.





















