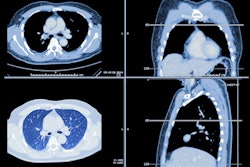
Stricter Lung-RADS categories in terms of nodule size help clinicians to categorize those found on follow-up lung cancer screening CT exams, according to a study by researchers from Harvard University. Their results were published November 10 in the American Journal of Roentgenology.
The results could help clinicians better triage pulmonary nodules, wrote Dr. Mark Hammer and Dr. Suzanne Byrne of Brigham and Women's Hospital and Harvard Medical School in Boston.
"With increasing use of CT lung cancer screening, algorithms to triage pulmonary nodules are critically important to provide optimal management of [lung cancer screening] patients," the two wrote.
Lung nodules found on screening CT are categorized using the Lung-RADS system or categories generated by the Dutch-Belgian Randomized Lung Cancer Screening (NELSON) trial. But nodules identified on follow-up screening may require a different approach than those found on baseline CT because they may have a higher risk of malignancy, the authors noted.
Nodule assessment algorithms such as those from the Fleischner Society and the NELSON trial use the same size cutoffs for new lung nodules on follow-up CT. But the Lung-RADS protocol recommends a lower size threshold (with the "clinical," or standard protocol setting the size for a suspicious nodule at ≥ 8 to < 15 mm and the stricter protocol setting it at 6 to > 8 mm).
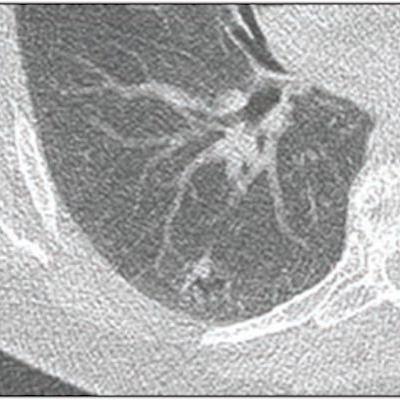
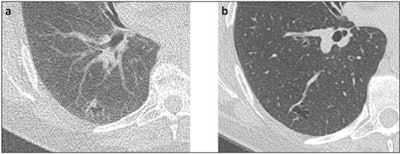 58-year-old woman with right lower lobe nodule. (a) Present lung cancer screening CT and (b) lung cancer screening CT performed 2 years prior. Nodule described as growing pure ground-glass nodule (associated with cystic lesion), measuring 15 mm in mean diameter. Nodule categorized Lung-RADS 3 by clinical report, though Lung-RADS 2 by strict application of size criteria. Subsequent wedge resection demonstrated lepidic-predominant adenocarcinoma. Images and caption courtesy of the AJR.
58-year-old woman with right lower lobe nodule. (a) Present lung cancer screening CT and (b) lung cancer screening CT performed 2 years prior. Nodule described as growing pure ground-glass nodule (associated with cystic lesion), measuring 15 mm in mean diameter. Nodule categorized Lung-RADS 3 by clinical report, though Lung-RADS 2 by strict application of size criteria. Subsequent wedge resection demonstrated lepidic-predominant adenocarcinoma. Images and caption courtesy of the AJR.Byrne and Hammer investigated the utility of both Lung-RADS algorithms for assessing new nodules found on follow-up CT. Their study included 185 follow-up CT lung cancer screening exams with nodules in 185 patients with available baseline exams. Of these 185 nodules, 56% were existing and 44% were new, with a median diameter of 7 mm; they were classified in the following Lung-RAD categories:
- 50 in category 2 (apparently benign)
- 45 in category 3 (probably benign)
- 47 in category 4A (additional diagnostic imaging recommended)
- 30 in category 4B (very suspicious)
- 13 in category 4X (also suspicious; additional features that increases suspicion)
Twenty-nine malignant nodules were identified out of the 185. Of these, 1% were found in stable existing nodules, 5% in new nodules, and 44% in growing existing nodules.
The study found the following regarding the two protocols' diagnostic performance:
| Diagnostic performance of two lung nodule assessment protocols | ||
| Measure | Clinical Lung-RADS (suspicious nodule size, ≥ 8 to < 15 mm) | Strict Lung-RADS (suspicious nodule size, 6 to > 8 mm) |
| Existing nodules | ||
| Sensitivity | 100% | 65% |
| Specificity | 94% | 98% |
| New nodules | ||
| Sensitivity | 100% | 74% |
| Specificity | 41% | 38% |
Although applying the stricter Lung-RADS framework to new nodules on follow-up CT didn't necessarily beat the clinical Lung-RADS framework for sensitivity and specificity, it did change the category for 59 of the 185 found, the pair noted:
- One category-2 nodule was changed to category 3.
- 29 category-3 nodules were changed to category 2, 4A, and 4B.
- 27 category-4B nodules were changed to category 2.
The net result of these adjustments was 83 nodules recategorized as Lung-RADS 2 using the stricter framework compared with 50 categorized as Lung-RADS 2, according to the clinical framework.
"Lung-RADS, as applied by radiologists in clinical practice, had excellent performance for cancer risk assessment on follow-up screening examinations ... [and] strict Lung-RADS criteria downgrades some malignancies," Byrne and Hammer concluded.