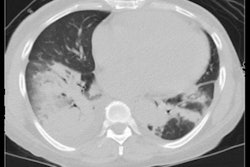
As the COVID-19 pandemic has progressed, chest CT has proved to be a valuable tool not only for diagnosing COVID-19 but also for predicting outcomes. On Sunday at RSNA 2021, investigators shared study results that further demonstrated CT's effectiveness for assessing disease severity and patients' risk of death.
How bad is it?
In the context of COVID-19, chest CT produces data that help clinicians assess a patient's mortality risk, Dr. Fatemeh Darvizeh of the IRCCS San Raffaele Scientific Institute in Milan, Italy, told session attendees. She and her colleagues found two biomarkers of cardiovascular risk to be associated with disease severity in COVID-19 patients: sarcopenia and fatty liver disease.
"The high rate of morbidity and mortality associated with COVID-19 infection raises the need to identify nonclinical parameters that can early stratify the patient's risk of death," she said. "In this context, chest CT -- already widely used for the evaluation of lung parenchyma -- can provide additional information, allowing a better risk stratification in individual patients."
Darvizeh's group conducted a study that included 1,669 patients who underwent noncontrast chest CT within 72 hours of hospital admission; the team collected clinical data such as patient demographics, comorbidities, and lab test results from electronic medical records, and tracked whether patients had received oxygen therapy or ICU care and whether they died in hospital.
The investigators assessed the chest CT exams for well-aerated lung volume, percentage of pneumonia involvement, coronary artery calcium scoring, paraverterbral muscle density as a marker of sarcopenia, bone density as a marker of osteoporosis, and liver density as a marker of liver steatosis. Of the patient cohort, 66.1% were male and 63.8% had comorbidities; 68.1% had less than 50% COVID-19 lung involvement on CT, while 31.9% had more than 50% lung involvement.
A quarter of the cohort died, with the mortality rate higher in men (28%) than in women (19%). Risk factors for COVID-19 mortality included older age, male sex, higher coronary artery calcium scores, higher degree of sarcopenia, liver steatosis, and lower bone density. Lung involvement of more than 50% raised a patient's odds of dying from COVID-19 more than three-fold.
Overall, the researchers found that sarcopenia and fatty liver on chest CT to be associated with the severity of COVID-19 pneumonia and outcome.
"Chest CT performed for diagnosis of COVID-19 pneumonia helps to identify new features in high-risk COVID patients," Darvizeh said. "An accurate analysis of chest CT is important not only for assessment of lung parenchyma, but also [for assessing] mortality risk of patients affected by COVID-19 at hospital admission."
CT + cytokines = better severity prediction
Presenter and third-year medical student Emma Klein of the Icahn School of Medicine at Mount Sinai in New York City shared results from a study that found that adding plasma cytokine data to chest CT results improves assessment of COVID-19 disease severity and mortality risk.
The team's research included 152 patients with COVID-19 who had plasma cytokine assessment and a chest CT within five days of hospital admission. The group evaluated the predictive value of five models:
- Cytokine data only
- CT qualitative data
- CT quantitative data
- A combination of data included in first three models
- An "optimized" model that included cytokine data, ground-glass opacities, aerated lung ratio, and age
| Power of 5 models for predicting COVID-19 severity and mortality by area under the curve (AUC) | |||||
| Factor | Cytokine model | CT qualitative model | CT quantitative model | Combined model | Optimized model |
| Degree of disease severity | 0.70 | 0.74 | 0.81 | 0.84 | 0.82 |
| Death | 0.70 | 0.61 | 0.66 | 0.75 | 0.78 |
The combination model proved most effective for assessing the degree of disease severity, while the optimized model was most effective for assessing mortality risk, the study authors found.
"CT imaging alone and in combination with cytokines may be helpful in predicting COVID-19 patient outcome," Klein concluded.