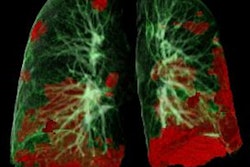
SARS-CoV-2 infection may lead to small-airways disease in the long term, which can lead to additional health complications for survivors of COVID-19, according to a study published March 15 in Radiology.
"The persistence of respiratory abnormalities ... raises concern for permanent airway remodeling and fibrosis following SARS-CoV-2 infection," wrote a team led by Dr. Josalyn Cho of the University of Iowa in Iowa City.
The SARS-CoV-2 virus and ensuing COVID-19 disease has been shown to cause pulmonary abnormalities that continue for weeks or months after the illness has resolved in more than 50% of adults, the group noted. But the lasting effects of these abnormalities remain unclear.
"The long-term effects of SARS-CoV-2 infection ... are poorly understood, but the potential impact on our healthcare system is enormous given the millions of infections worldwide, most of [which were] mild disease," the investigators wrote. "We hypothesized that SARS-CoV-2 infection leads to small airways disease, as has been observed in other severe respiratory viral infections."
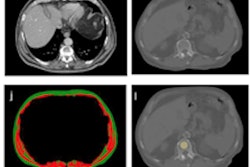
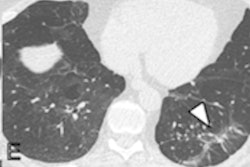
The study included 100 patients with confirmed COVID-19 who had ongoing symptoms more than 30 days after diagnosis and 106 healthy controls. Patients were categorized as ambulatory (67%), hospitalized (17%), or requiring intensive care (16%); the team gathered information on symptoms, pulmonary function tests, and chest CT imaging for each individual. Patients were imaged on chest CT using an expiratory protocol, a postexhalation scan that helps assess air trapping.
The most common chest CT findings in patients experiencing postacute sequelae of COVID-19 were air trapping (58%) and ground-glass opacities (51%); ground-glass opacities were more common among patients who required hospitalization in the intensive care unit (ICU) (94%) compared with ambulatory patients (36%).
The mean percentage of total lung area affected by air trapping post-COVID-19 was comparable across disease severity categories, with 25.4% of ambulatory patients, 34.6% of hospitalized patients, and 27.3% of intensive care patients experiencing the condition. In contrast, mean percentage of total lung affected by air trapping post-COVID-19 was only 7.5% in the healthy control group.
The group also found that at least one coexisting disease was present in 67% of participants with postacute sequelae of COVID-19, with obesity and hypertension the most common; the most common pulmonary condition in these patients was asthma.
"If a portion of patients continues to have small airways disease [post COVID-19], then we need to think about the mechanisms behind it," senior study author Dr. Alejandro Comellas, also of the University of Iowa, said in a statement released by the RSNA. "It could be something related to inflammation that's reversible, or it may be something related to a scar that is irreversible, and then we need to look at ways to prevent further progression of the disease."