Head CT shows that antithrombotics don't boost incidence of brain bleeds in patients who have sustained a ground-level fall -- though they may cause the hematoma to expand, according to March 24 research published in the American Journal of Roentgenology.
The findings could help clarify whether follow-up CT is indicated in patients who have fallen and are also on antithrombotics, wrote a team led by Dr. Zeynep Vardar of the University of Massachusetts Medical Center in Worcester.
"Various imaging recommendations have been suggested for patients with antithrombotic use who present with trauma," the team wrote. "Some authors recommend imaging regardless of whether the patient experiences loss of consciousness or amnesia, while others suggest avoiding imaging in anticoagulated patients who have normal Glasgow coma scale and no focal neurologic deficit."
Ground-level falls are common in older people, with an incidence of 30% per year in those over 65 and 50% in those over 80, the team explained. Combine this propensity with the fact that elderly people are also more likely to be taking antithrombotic medication, and it's no wonder that emergency departments are treating more patients who have fallen and are also on antithrombotics.
"Ground-level fall is traditionally considered to represent low-energy trauma that is potentially associated with minor head trauma," the researchers wrote. "However, minor head trauma may lead to substantial head injuries in patients on antithrombotic therapy, for example causing traumatic intracranial hemorrhage (tICH) by either direct impact or indirect force."
Vardar and colleagues sought to assess the frequency of traumatic head injury in patients on antithrombotic medication presenting in the emergency department after a ground-level fall (Glasgow Coma Scale ≥ 14 and no nerve, spinal, or brain function deficit). The study included 1,630 patients who underwent head CT scans due to a fall between January and December 2020. The head CT exams were reviewed for brain bleeds; any follow-up exams were reviewed for hematoma expansion.
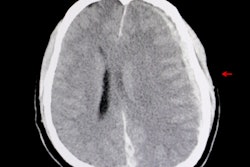
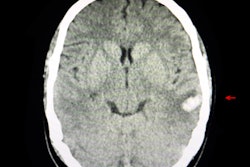
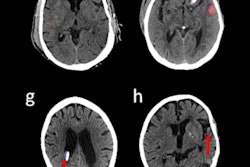
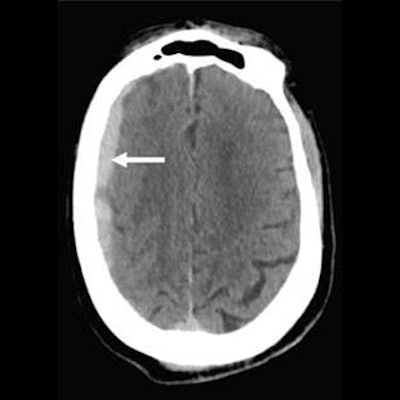
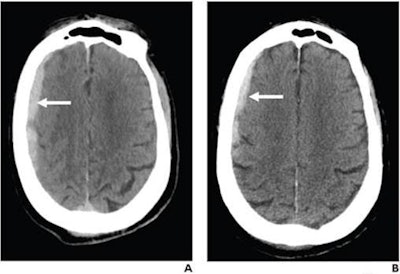 76-year-old patient, not on antithrombotic therapy, presenting to emergency department after ground-level fall (Glasgow Coma Scale of 15). Patient had no focal neurological deficit. (A) Axial slice from initial noncontrast head CT shows right frontoparietal subdural hematoma (arrow); hematoma was classified as exhibiting both regional mass effect and midline shift (not shown). (B) Axial slice from noncontrast head CT performed eight hours later shows stable size of hematoma (arrow). Patient was discharged home in stable condition two days later. Images and caption courtesy of the American Roentgen Ray Society.
76-year-old patient, not on antithrombotic therapy, presenting to emergency department after ground-level fall (Glasgow Coma Scale of 15). Patient had no focal neurological deficit. (A) Axial slice from initial noncontrast head CT shows right frontoparietal subdural hematoma (arrow); hematoma was classified as exhibiting both regional mass effect and midline shift (not shown). (B) Axial slice from noncontrast head CT performed eight hours later shows stable size of hematoma (arrow). Patient was discharged home in stable condition two days later. Images and caption courtesy of the American Roentgen Ray Society.The group found that frequency of brain bleeds in patients who had experienced these types of falls but had good neurological status on presentation to the emergency department did not differ significantly between individuals on antithrombotic therapy and those not on it (4.4% vs. 3.1%, p = 0.24). But patients on antithrombotic medication did have increased incidence of hematoma expansion on follow-up head CT compared to those who were not on the medication (26.2% vs. 4.8%, p = 0.04).
The results may help clarify which patients need follow-up head CT in this situation, the authors noted.
"[Our] findings suggest adopting similar strategies for initial imaging evaluation by head CT in the two groups [i.e., those patients who are on antithrombotics and those patients who are not]," they wrote. "However, while early follow-up head CT should be routinely performed in patients on antithrombotic therapy with tICH systemic early imaging follow up may not be required in patients with tICH not on antithrombotic therapy."