Photon-counting CT (PCCT) visualizes cerebrospinal fluid (CSF) venous fistula (CVF) better than traditional imaging approaches such as CT myelography or MRI, according to a report published April 18 in JAMA Neurology.
The findings could translate to better diagnosis and treatment of CVF, which can cause lower than normal fluid pressure inside the skull (also known as spontaneous intracranial hypotension, which is typically treated with epidural blood patches), wrote a team led by Dr. Fides Schwartz of Duke University in Durham, NC.
"Epidural blood patches are the standard treatment for spontaneous intracranial hypotension ... [and] some studies suggest that targeting a visualized leak or CVF improved efficacy [of this treatment from 52% to 87%]," the group noted.
Cerebrospinal fluid venous fistula can be difficult to visualize, the group explained. Typically, CT myelography or MRI are used to diagnose spontaneous intracranial hypotension -- and thus CVF -- but these modalities don't necessarily identify the site of the fistula, which can be found anywhere along the axis of the central nervous system and is usually no more than 1 mm to 2 mm wide, the group explained.
That's where photon-counting CT (PCCT) shows promise. Photon-counting CT is based on dual-energy x-ray tubes and photon-counting detectors that distinguish photon energy in the x-ray beam -- which reduces image noise, improves signal, and can increase spatial resolution from 0.6 mm to 0.2 mm, Schwartz and colleagues wrote.
"At our institution, this has been demonstrated to lead to better diagnostic quality of skull base imaging, where the structures of the inner and middle ear can be more confidently evaluated with high-resolution imaging," they reported.
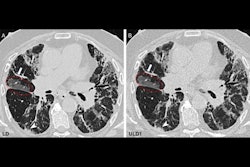
The researchers shared images of a CVF that occurred in a 56-year-old woman and was visualized with both standard CT myelography and with photon-counting CT. CT myelography could not confirm CVF, but the photon-counting image could -- which led to better-tailored treatment.
 Coronal 3-mm maximum intensity projection image of a CSF-venous fistula (arrow indicates the iodinated contrast in the fistula). This was not detected on regular clinical CT with a 0.6-mm resolution but was clearly depicted on a newly U.S. Food and Drug Adminstration-approved photon-counting CT scanner with 0.2-mm resolution. Images and caption courtesy of Dr. Fides Schwartz.
Coronal 3-mm maximum intensity projection image of a CSF-venous fistula (arrow indicates the iodinated contrast in the fistula). This was not detected on regular clinical CT with a 0.6-mm resolution but was clearly depicted on a newly U.S. Food and Drug Adminstration-approved photon-counting CT scanner with 0.2-mm resolution. Images and caption courtesy of Dr. Fides Schwartz."We had only hoped for this new technology to be able to depict these very small structures better than the current clinical standard and were very excited to actually see how the higher spatial resolution of 0.2 mm in combination with the material decomposition capabilities were improving our diagnostic capabilities," Schwartz told AuntMinnie.com.
Since photon-counting CT is still new, it will likely take some time to integrate it into clinical practice, Schwartz said.
"Implementation of photon-counting CT scanners is a clinical challenge, as the scanning protocols need to be adapted from current scanners to unlock the full potential of this new technology," she said. "In addition, optimization of reconstruction kernels and image display in PACS systems is needed, to make the best use of the photon-counting scanners' capabilities."
But the study results are promising, according to the team.
"The PCCT scanner has the capability of depicting cerebrospinal fluid venous fistula better than standard clinical imaging," the authors concluded. "[Our] work marks an important advancement in radiology diagnostics and may result in improved patient care with better fistula detection and more targeted treatments for spontaneous intracranial hypotension."