Radiologists using a visual ordinal scoring scale to evaluate coronary artery calcium (CAC) performed just as well on general chest CT studies as they did on dedicated cardiac CT exams, according to a study published April 27 in the American Journal of Roentgenology.
The study results suggest that clinicians could identify more patients at risk of heart disease on chest CT exams performed for any indication, not just cardiac, wrote a team led by Dr. Camila Fresno of the University of Toronto in Canada.
"Routine reporting of CAC on all chest CT studies ... could have a large clinical impact given that over 90 million CT studies are performed annually in the United States," the group noted. "Visual ordinal scoring of CAC on chest CT is an example of opportunistic CT screening, which leverages robust data embedded within images that are unrelated to the study's specific clinical indication."
Atherosclerotic cardiovascular disease is the leading cause of death in the U.S., and coronary artery calcium (CAC) is a strong determining factor for predicting adverse event risk, the group explained. Incidental CAC can be found on nongated chest CT that patients undergo for other indications, and radiologists' visual assessment of CAC on these nongated exams has been shown to correspond to Agatston scores.
But more research is needed to determine the diagnostic performance, outcome prediction, and reader agreement of visual evaluation of CAC on both contrast-enhanced and nongated, noncontrast chest CT.
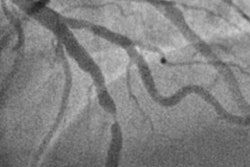
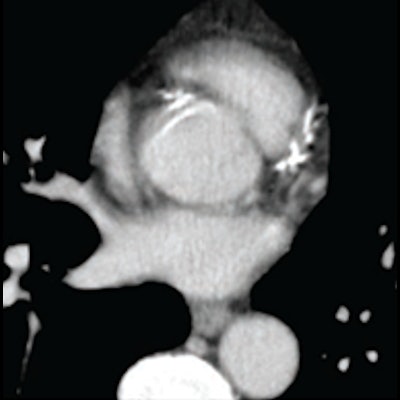
To this end, Fresno and colleagues conducted a study that included 260 patients who underwent nongated chest CT for indications besides CAC assessment (of these, 116 had contrast-enhanced exams and 144 had exams without contrast) and a cardiac calcium score CT within a 12-month period. A cardiothoracic radiologist scored CAC on chest CT using a visual ordinal assessment that consisted of the following: absent (0), mild (1 to 99), moderate (100 to 299), or severe (> 300).
 (A) mild, (B) moderate, (C) severe CAC on nongated contrast-enhanced chest image. Image and caption courtesy of the American Journal of Roentgenology.
(A) mild, (B) moderate, (C) severe CAC on nongated contrast-enhanced chest image. Image and caption courtesy of the American Journal of Roentgenology.CAC was also evaluated with software that calculated volume across all identified plaque and produced a total Agatston score. To determine reader agreement between the visual assessment and cardiac CT results, a second radiologist evaluated a subset of 50 chest CT exams.
Fresno and colleagues found that radiologist visual assessment of CAC on both contrast-enhanced and noncontrast chest CT had comparable sensitivity, specificity, and positive predictive value compared with cardiac CT as the reference standard, demonstrated by a lack of statistical significance.
| Diagnostic performance of radiologist visual assessment of chest CT with cardiac CT as reference standard | |||
| Contrast- enhanced CT | Noncontrast CT | p-value (compared with cardiac CT results) | |
| Any CAC | |||
| Sensitivity | 83% | 90% | 0.20 |
| Specificity | 100% | 100% | 0.99 |
| Positive predictive value | 100% | 100% | 0.99 |
| Negative predictive value | 76% | 83% | 0.34 |
| Moderate to severe CAC | |||
| Sensitivity | 72% | 67% | 0.61 |
| Specificity | 99% | 99% | 0.99 |
| Positive predictive value | 97% | 97% | 0.96 |
| Negative predictive value | 82% | 86% | 0.55 |
The group measured reader agreement using the Kappa coefficient, and found that visual ordinal assessment of coronary artery calcium was 0.89 on contrast-enhanced CT and 0.95 on noncontrast, nongated chest CT.
"Routine reporting of CAC on all chest CT examinations regardless of clinical indication and contrast material administration could identify a substantial number of patients without known atherosclerotic cardiovascular disease who may benefit from preventive treatment," the authors concluded.