Men with lung cancer have a much higher risk of mortality compared with women, says a new paper published August 1 in Lung Cancer. But this difference disappears if they got CT lung screening, suggesting that screening can even out gender disparities.
Researchers found that among individuals with lung cancer who got screened and those who didn't, men had a 62% higher mortality rate than females. But there was no statistically significant difference in mortality rates between men and women when data was analyzed based on who got screened and who didn't.
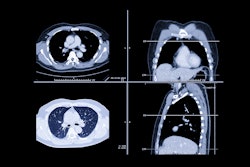
CT lung screening has been demonstrated to reduce mortality by 20% among high-risk individuals like heavy smokers. But much of the recent research into CT lung cancer screening has focused on racial and gender disparities in screening.
For example, a July 24 paper in Cancer Medicine found that while the recent expansion of CT lung screening guidelines doubled the number of eligible individuals, many might not be able to get to a screening facility due to socioeconomic factors. And a July 28 study in JAMA Oncology questioned whether existing guidelines are missing many at-risk people.
With respect to women, part of the problem with recent research is that females have been somewhat underrepresented. The landmark National Lung Screening Trial consisted of 59% males versus 41% females, while the Dutch-Belgian Lung Cancer Screening (NELSON) saw an even greater disparity, with only 16% of participants being women. At the same time, the incidence of lung cancer has fallen 35% in men over the last four decades, but it has increased 87% in women.
In the current study, a team led by Adriana Rodriguez Alvarez of Boston University wanted to focus more closely on gender disparities in CT lung screening. The group analyzed data from the Boston Lung Cancer Study acquired from 2013-2021. In all, 1,216 individuals diagnosed with lung cancer were included in their analysis; of these, 9.4% had undergone CT lung cancer screening.
The researchers separated the study subjects into four groups, defined by gender and screening status. They also classified individuals by stage of cancer at diagnosis. Alvarez and colleagues then used propensity score matching to create a study cohort that was balanced between men and women.
They found that the only category with a statistically significant difference was in mortality rates for men versus women in the group that included both screened and unscreened individuals.
| Lung cancer mortality by CT lung cancer screening status and gender | ||
| Screening status and gender | Hazard ratio for mortality | p-value |
| Men vs. women (screened and unscreened) | 1.62 | p = 0.00022 |
| Screened -- all genders (vs. unscreened) | 1.14 | p = 0.79 |
| Unscreened men (vs. unscreened women) | 1.6 | p = 0.54 |
| Screened men (vs. screened women) | 0.57 | p = 0.46 |
In other findings, the researchers noted that early-stage cancer (stage 1A) was the most common diagnosis in the screened individuals, while late-stage cancer (stage IV) and extensive-stage cancer were more common in those who were not screened. Also, 27.5% of unscreened men died, versus 17.8% of unscreened women.
The researchers noted that their findings correlated with previous studies that pointed to a better prognosis for women with lung cancer than men, particularly with those who were not screened. But the difference disappeared among those who were screened.
"However, when screened women were compared to screened men, there were no differences in survival probability," the authors concluded. "These findings could suggest that screening, regardless of sex, is effective to reduce sex disparities in lung cancer survival."