A technique called texture analysis used with CT pulmonary angiography (CTPA) imaging could help clinicians assess the prognosis of patients with acute pulmonary embolism (PE), a study published August 16 in Angiology has found.
The results may translate into better patient care by providing a clearer sense of the severity of a patient's condition, wrote a team led by Dr. Jakob Leonhardi of the University of Leipzig in Germany.
"There is no doubt that images analyzed with texture analysis can provide insight into the microstructure of the embolus," the group noted.
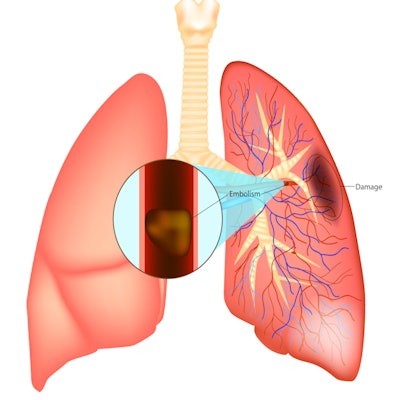
Pulmonary embolism is a serious condition, with 30-day mortality rates that range from 0.5% to 20%. CT pulmonary angiography is the standard tool for diagnosing PE, and it has high sensitivity and specificity.
But it can still be improved, and texture analysis is an emerging technique for this use, the study authors explained. By analyzing the texture of a thrombus, the technique can identify quantitative biomarkers and can offer more information than a radiologist reader can alone.
"Texture analysis ... can provide information from different images, which is beyond the scope of the clinical observation carried out by a radiologist," Leonhardi and colleagues explained.
For example, texture analysis could predict the permeability of a thrombus -- this could help clinicians determine whether to use mechanical thrombectomy to remove the thrombus. But despite these possible advantages, texture analysis has not been widely used for pulmonary embolism.
Leonhardi's team conducted a study that included 216 patients, all of whom underwent CT imaging. The group then used MaZda, free texture analysis software developed at the Institute of Electronics, Technical University of Lodz in Poland, on axial slices of contrast-enhanced CTPA exams. A region of interest was drawn around the margin of the embolus, and a total of 279 texture features were analyzed for each patient. The group also tracked clinical scores, blood parameters, need for intubation, admission to the intensive care unit (ICU), and mortality rates of the patient cohort.
Of the 216 individuals who participated in the study, 26.4% (57) died; 79.6% (172) were admitted to the ICU, and 25.8% (56) showed signs of deep venous thrombosis. Other patient characteristics included the following:
- 27.2% had active malignant disease.
- 23.%% had undergone surgery four weeks before having the CTPA scan.
- 11.9% had chronic lung disease.
- 17.9% had chronic heart failure.
The group found association in texture differences between mortality in days with a few texture difference parameters, such as SumVarnc (i.e., sum variance, p < 0.001), and with AngScMom (i.e., angular second moment), which correlated with patients' sepsis-related organ failure assessment score (p < 0.001). The authors also found significant differences between texture features among survivors and nonsurvivors and in patients who needed ICU care and those who did not (p = 0.02).
Texture analysis shows promise for adding useful data to the workup of patients presenting with pulmonary embolism, according to the investigators.
"Several texture features of pulmonary emboli derived from CTPA were associated with mortality, need for ICU admission, clinical and serological parameters in patients with acute PE," they concluded. "This highlights the possible clinical benefit of those novel imaging biomarkers."





















