A CT-based assessment tool shows that recanalization is an effective way to preserve functional outcomes long term in stroke patients -- even at later time windows after the event, a team of German researchers has found.
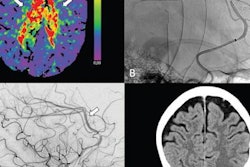
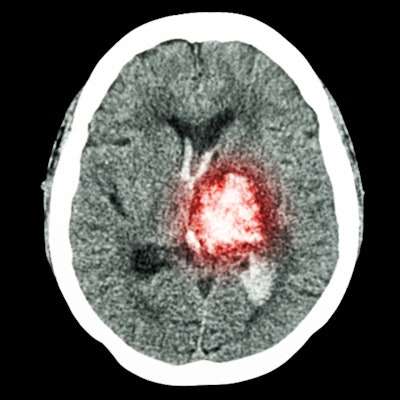
The tool, called the Alberta Stroke Program Early CT Score (ASPECTS), is a 10-point scale that uses data from a baseline noncontrast CT scan to evaluate the extent of the infarction; scores under 5 indicate a larger infarct area. A group led by Dr. Gabriel Broocks of University Medical Center Hamburg-Eppendorf in Germany found that patients with low ASPECTS scores (3 to 5) responded well to vessel recanalization for up to almost 18 hours after stroke onset -- a much longer timeframe than typically assumed. The research was published October 14 in JAMA Network Open.
"The findings of this study suggest that endovascular treatment for patients with ischemic stroke and extensive signs of infarction who present in the extended time window was associated with better functional outcomes," the group noted.
The efficacy of ASPECTS for helping to determine how best to treat stroke patients has been under consideration recently. In fact, earlier this month, Japanese researchers published findings that showed ASPECTS can help clinicians evaluate the scope of damage and determine whether the patient will benefit from endovascular treatment. But other research has not definitively shown how patients with lower ASPECTS scores -- and thus, larger infarct areas -- respond to treatment after longer times post-stroke, Broocks and colleagues wrote.
The team conducted a study that included 285 patients enrolled in the German Stroke Registry-Endovascular Treatment trial between July 2015 and December 2019 who presented between six and 24 hours after onset of the stroke, underwent CT and were determined to have an ASPECTS score of 5 or less, and had endovascular treatment. Primary outcome for the research was a modified Rankin scale (mRS) score of 3 or less 90 days after the stroke event, indicating successful recanalization (i.e., restored flow to the affected brain vessels) via endovascular treatment. According to mRS scoring, lower scores correlate to better patient outcomes.
Of the study cohort, 28% had an mRS score of 3 or less at 90 days post-stroke, and this was more common among patients with successful recanalization than those without. The overall rate of functional independence among the study cohort at 90 days post-stroke was 20%.
Successful revascularization among stroke patients with low ASPECTS scores translated to better outcomes (measured by mRS score).
| Recanalization outcomes in patients with mRS score of 3 at 90-days post-stroke | |||
| Measure | Unsuccessful recanalization | Successful recanalization | |
| Favorable overall | 13% | 32% | |
| Functional independence overall | 9% | 23% | |
| Functional independence among patients older than 75 | 11% | 16% | |
The study findings are good news for stroke sufferers.
"[Our study] revealed [that] the rate of favorable outcomes after successful endovascular recanalization among this patient cohort was similar to previously reported outcomes among patients with low ASPECTS in the early time window, suggesting that patients with large core infarcts may benefit even in the extended time window," the authors concluded.