A deep-learning model trained to measure total lung capacity on x-rays could help clinicians manage patients with idiopathic pulmonary fibrosis (IPF), according to a study published October 25 in Radiology.
Researchers at Seoul National University Hospital in Korea developed a deep-learning algorithm to estimate total lung capacity (TLC) on chest x-rays. In a test set of patients with IPF, greater TLC estimated by the algorithm was associated with better patient survival, they found.
"A fully automatic, deep learning-based model estimated total lung capacity from chest radiographs, and the model predicted survival in idiopathic pulmonary fibrosis," wrote a team led by Dr. Hyungjin Kim.
A reduction in lung volume is a hallmark of idiopathic pulmonary fibrosis. Currently, the most accurate measurement requires a technically difficult procedure with use of a total body plethysmograph, a well-trained technician, and a cooperative patient, according to the authors.
Conversely, TLC estimated by an artificial algorithm on chest x-rays could be used as a digital screening test or as a monitoring tool in patients with respiratory symptoms or signs, they wrote.
For the study, the investigators first trained a deep-learning model to measure TLC using 50,000 consecutive chest CT scans performed between January 2015 and June 2017 at their institution. They then fine-tuned the algorithm on 3,523 pairs of posteroanterior chest radiographs and plethysmographic TLC measurements from consecutive patients who underwent pulmonary function testing on the same day. To test the model, they used data sets from two tertiary care centers and one from a community hospital that included 217 patients with IPF.
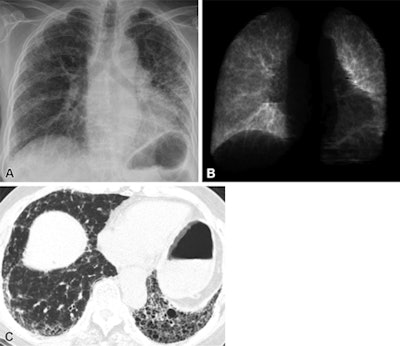 Images of a 72-year-old woman with idiopathic pulmonary fibrosis with an estimated total lung capacity of 2.96 L. (A) Posteroanterior chest radiograph; (B) the corresponding segmented lungs of the chest radiograph; and (C) unenhanced axial chest CT scan. The patient died 20.3 months after the date of the chest radiograph. Image courtesy of Radiology.
Images of a 72-year-old woman with idiopathic pulmonary fibrosis with an estimated total lung capacity of 2.96 L. (A) Posteroanterior chest radiograph; (B) the corresponding segmented lungs of the chest radiograph; and (C) unenhanced axial chest CT scan. The patient died 20.3 months after the date of the chest radiograph. Image courtesy of Radiology.The group found that the difference between TLC on the x-ray images and those estimated by the algorithm were small (0.69 liters vs. 0.73 liters) in the first external test set, and 0.52 liters and 0.53 liters in the second external test set. In the imaging set of 217 patients with IPF, a greater estimated TLC was associated with lower mortality risk (adjusted hazard ratio, 0.97 per percent, p = 0.001), the team found. In the imaging set of 217 patients with IPF, greater estimated TLC percentage was associated with lower mortality risk (adjusted hazard ratio, 0.97 per percent, p = 0.001).
"Our proposed method, which is a fully automatic end-to-end algorithm, does not necessitate planimetric techniques or manual linear measurements for TLC estimation," Kim and colleagues wrote.
In an accompanying editorial, Ronald Sorkness, PhD, a pulmonary physiologist and professor emeritus at the University of Wisconsin-Madison, wrote that the results are intriguing, and the concept is worth further development.
"If a quick, easy, low-risk image could be obtained with the patient in an upright position for TLC measurement, such an approach could be a valuable addition to the routine chest radiography and an alternative to plethysmography," he wrote.