CHICAGO - Can low-dose CT lung cancer screening go even lower? Perhaps not, according to research presented November 29 at the RSNA meeting in Chicago.
Even though low-dose CT (LDCT) lung cancer screening radiation dose could be further reduced, doing so may not be beneficial, Dr. Matheus Zanon of Hospital São Lucas da PUCRS in Porto Alegre, Brazil, and colleagues found.
"Although the mean effective radiation dose dropped to almost a third from low-dose CT to ultra-low-dose CT, interreader agreement was poor for significant findings, such as consolidation and GGO, that may represent other types of lung cancer," the group wrote.
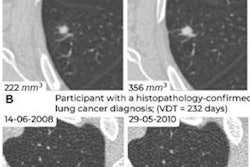
Low-dose CT lung cancer screening has been shown to effectively reduce mortality rates, primarily from identifying disease early. And although the exam imparts smaller doses of radiation than other CT studies might, the question of whether these doses can be reduced even further remains.
Zanon's group compared the performance of ultralow-dose CT (0.39 mSv) and low-dose CT (1.2 mSv) for lung cancer screening among 265 smokers eligible for the exam according to 2021 U.S. Preventive Services Task Force (USPSTF) guidelines (i.e., individuals between the ages of 50 and 80 with a 20 pack-year smoking history and who are current smokers or former smokers who quit within the past 15 years). Patients underwent both ultralow-dose and low-dose CT studies and two radiologists evaluated the images for consolidation, ground-glass opacity, septal thickening, pulmonary nodules, bronchial wall thickening, pleural effusion, emphysema, bronchiectasis, and atelectasis.
Of the 258 patients, 58, or 21.9%, had abnormal CT scans. The mean effective radiation doses for low-dose and ultralow-dose CT exams were 1.2 mSv and 0.39 mSv respectively, for a dose reduction of 67.8%.
The investigators measured interreader agreement using kappa coefficient values. Kappa value was high for emphysema (0.92) and nodules (0.91); strong for bronchial wall thickening, bronchiectasis, and atelectasis (range, 0.8 to 0.9); and "substantial" for consolidation, septal thickening, and pleural effusion (range, 0.6 to 0.8). However, agreement for ground-glass opacities was poor (kappa, 0.37).
"Despite the exciting agreement for some pulmonary findings, these results [call into] question whether using an ultra-low-dose protocol for lung cancer screening would be adequate, as many subsolid or ground-glass opacity lesions could be missed," Zanon and colleagues concluded. "Also, despite the significant reduction in the [mean effective radiation dose] it is questionable whether there is a patient benefit from going to 1.2 mSv to 0.39 mSv."