Contrast-enhanced CT (CECT) can help assess response to intra-arterial treatment in patients with neuroendocrine liver metastases and predict survival outcomes, according to a study published on January 6 in Radiology: Imaging Cancer.
CECT does this by allowing clinicians to track patients' liver-enhancing tumor burden (LETB), wrote a team led by Dr. Jessica Assouline of the University of Paris in France.
"Volumetric tumor enhancement assessment has been shown to help predict survival in patients with cancer," the group noted. "[But] rather than a lesion-by-lesion volumetric analysis, volumetric assessment of metastatic disease in the entire liver, also known as the liver enhancing tumor burden, is a more comprehensive marker of tumor response in neuroendocrine liver metastases after intra-arterial treatments."
Predicting patient outcomes after intra-arterial treatment for liver metastases -- such as transarterial embolization or chemoembolization -- can be tricky, Assouline and colleagues explained. Previous studies have used MRI to investigate a volumetric assessment of LETB after treatment even though in clinical practice, CT is often used for this purpose, they wrote.
The team sought to evaluate CT's efficacy for this indication, conducting a study that included 119 patients with neuroendocrine liver metastases who underwent 161 intra-arterial procedures between April 2006 and December 2018. The group evaluated treatment response using the Response Evaluation Criteria in Solid Tumors (RECIST) and modified RECIST (mRECIST) tools, as well as the level of LETB on contrast-enhanced CT imaging, tracking patients' overall survival, recording the time from initial treatment until the time when intra-arterial treatments were considered untenable, and calculating hepatic and whole-body progression-free survival.
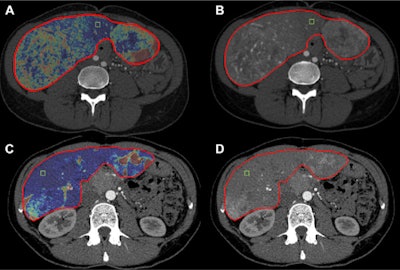 Changes in liver-enhancing tumor burden (LETB) in a 36-year-old woman with pancreatic neuroendocrine liver metastases treated with transarterial chemoembolization. (A, B) Pretreatment CT showed a total hepatic volume of 2823 cm3, a volume of enhancing tumor of 1035 cm3, and a LETB of 36.6%. (C, D) Post-treatment CT showed a total hepatic volume of 1607 cm3, a volume of enhancing tumor of 354 cm3, and an LETB of 22%. LETB dropped by 41%. Hepatic and whole-body progression-free survivals were each 11 months, and overall survival was 21 months. Note: The segmentation mask to determine the whole-liver volume is shown as the red borders of the liver. The green box represents the 0.5 cm3 region of interest placed in the nontumoral liver parenchyma to quantify the LETB. Images and caption courtesy of the RSNA.
Changes in liver-enhancing tumor burden (LETB) in a 36-year-old woman with pancreatic neuroendocrine liver metastases treated with transarterial chemoembolization. (A, B) Pretreatment CT showed a total hepatic volume of 2823 cm3, a volume of enhancing tumor of 1035 cm3, and a LETB of 36.6%. (C, D) Post-treatment CT showed a total hepatic volume of 1607 cm3, a volume of enhancing tumor of 354 cm3, and an LETB of 22%. LETB dropped by 41%. Hepatic and whole-body progression-free survivals were each 11 months, and overall survival was 21 months. Note: The segmentation mask to determine the whole-liver volume is shown as the red borders of the liver. The green box represents the 0.5 cm3 region of interest placed in the nontumoral liver parenchyma to quantify the LETB. Images and caption courtesy of the RSNA.Contrast-enhanced CT showed the following:
- A median reduction in LETB of 25.8% was the best indicator of overall survival, increasing survival outcomes from 51 months to 83 months and whole-body progression-free survival from eight months to 18 months.
- A 10% decrease in LETB best predicted time to when intra-arterial treatment would be unfeasible, from 12 months in patients unresponsive to treatment to 32 months in responsive patients. This percent decrease also translated to better hepatic progression-free survival outcomes, ranging from eight months to 18 months.
- Neither the RECIST nor the mRECIST tools helped predict patient outcomes, the group noted.
The study findings could give clinicians and their liver cancer patients a better idea of how effective treatment will be, according to the authors.
"Our study shows that early assessment of CT response according to LETB change helps predict survival outcome in patients with neuroendocrine liver metastases after intra-arterial treatments, with better discrimination than RECIST and mRECIST between responders and nonresponders," the group concluded.