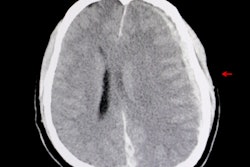
Of seven head CT findings in patients with traumatic brain injury (TBI), three in particular -- sulci/gyri effacement, midline shift, and cerebral peduncle effacement -- predict the need for neurosurgical intervention, researchers have found.
The results offer emergency physicians a way to quickly assess how best to manage TBI patients, wrote a team led by Soroosh Noorbakhsh, MD, of the University of Tennessee Health Science Center in Memphis. Noorbakhsh and colleagues published their findings October 4 in American Surgeon.
"[Our] schema may help predict need for intervention and expedite management of moderate to severe TBI," the group noted.
Traumatic brain injury demands rapid treatment to avoid secondary injury or death. The team investigated whether a simple protocol for quick interpretation of head CT exams by trauma surgeons and residents could help them predict a patient's need for neurosurgical intervention -- or risk of death -- from traumatic brain injury within 24 hours.
The researchers conducted a review of 444 patients with traumatic brain injury who presented in the emergency room in 2020 with a Glasgow Coma Scale (GCS) of 12 or less. (Scores of three to eight are considered severe; nine to 12, moderate; and 13 to 15 are considered mild TBI, or concussion.) Trauma surgeons and trainees each evaluated patients' head CT exams, scoring findings as normal or abnormal. The study's primary outcome was whether a patient underwent brain surgery or died within 24 hours.
The investigators assessed the following seven head CT findings from patients with traumatic brain injuries:
- Cerebrospinal fluid at foramen magnum
- Open fourth ventricle
- Cerebrospinal fluid around quadrigeminal plate
- Cerebrospinal fluid around cerebral peduncles
- Absence of midline shift
- Visible sulci/gyri
- Gray-white differentiation
Of the 444 patients, 21.4% underwent neurosurgery or died within 24 hours. Resident exam readers found that 5.8% of patients without any abnormal findings on head CT had surgery or died in the time period compared with 52% of those who had at least one abnormality. Trauma surgeons found that 8.7% of patients without any abnormal findings on head CT had surgery or died in the time period, compared with 54.9% of those who had at least one abnormality. Findings that indicated the highest risk for surgery or death from TBI were sulci/gyri effacement, midline shift, and cerebral peduncle effacement, the group reported.
In fact, Noorbakhsh and colleagues reported that when at least one or more of these seven head CT findings were abnormal, the sensitivity of readers' prediction of the need for surgery or risk of death was 78%, specificity was 81%, and negative predictive value was 93.1%.
"Any single abnormality in this schema significantly predicted a large increase in neurosurgical intervention/death in 24 hours in TBI patients, and three particular findings were most predictive," the authors concluded.
The complete study can be found here.