Diagnosing early-stage lung cancer with low-dose CT (LDCT) translates to a 20-year survival rate of 81%, according to a large-scale, 20-year international study published November 7 in Radiology.
And this survival rate is even higher among those diagnosed with Stage 1 disease, at 95%, lead author Claudia Henschke, MD, PhD, of the Icahn School of Medicine at Mount Sinai in New York City said in an RSNA statement.
"[Our study] is the first time that 20-year survival rates from annual screening have been reported," she said. "This 20-year survival rate of 81% is the estimated cure rate of all participants with lung cancers diagnosed by annual screening. This is a huge benefit compared to waiting for a diagnosis that, in usual care, is symptom-prompted."
Lung cancer is the primary cause of cancer death in the U.S., and the average lung cancer survival rate is 18.6%, according to the American Lung Association. Only 16% of lung cancers are caught at an early stage, according to the RSNA. And although treatments for advanced lung cancer have become more effective, the best way to reduce mortality is to catch the disease early through LDCT.
Henschke and colleagues have been studying the effectiveness of low-dose CT screening for lung cancer since 1992 and created the International Early Lung Cancer Action Program (I-ELCAP) -- an initiative that has included more than 89,000 participants in 80 institutions around the world. In 2006, the team assessed the 10-year survival rate of patients diagnosed with lung cancer on LDCT, finding a rate of 80%. This current analysis shows similar results.
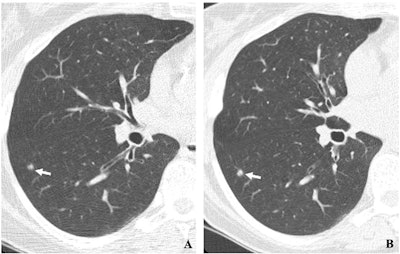 (A, B) Two annual repeat low-dose CT scans in a woman who was 60 years old at baseline enrollment in 1999. At baseline enrollment, she was currently smoking and had a 30-pack-year smoking history. No nodules were identified on baseline low-dose CT scans. On the sixth annual low-dose CT scan (B), a right lower lobe solid nodule (arrow) measuring 4.5 mm in maximum diameter was identified. The nodule could be identified in retrospect on the prior annual CT scan (arrow in A), when it measured 2 mm in maximum diameter. Estimated tumor volume doubling time was 161 days. Lobectomy was performed two months later, and diagnosis of stage 1aN0M0 moderately differentiated adenocarcinoma measuring 6 mm in maximum diameter was made. Expert pathologic panel review (22) of the pathologic specimen updated the diagnosis to adenocarcinoma with mixed subtype (80% acinar, 20% bronchoalveolar carcinoma components) with 5 mm of invasion. Images and caption courtesy of the RSNA.
(A, B) Two annual repeat low-dose CT scans in a woman who was 60 years old at baseline enrollment in 1999. At baseline enrollment, she was currently smoking and had a 30-pack-year smoking history. No nodules were identified on baseline low-dose CT scans. On the sixth annual low-dose CT scan (B), a right lower lobe solid nodule (arrow) measuring 4.5 mm in maximum diameter was identified. The nodule could be identified in retrospect on the prior annual CT scan (arrow in A), when it measured 2 mm in maximum diameter. Estimated tumor volume doubling time was 161 days. Lobectomy was performed two months later, and diagnosis of stage 1aN0M0 moderately differentiated adenocarcinoma measuring 6 mm in maximum diameter was made. Expert pathologic panel review (22) of the pathologic specimen updated the diagnosis to adenocarcinoma with mixed subtype (80% acinar, 20% bronchoalveolar carcinoma components) with 5 mm of invasion. Images and caption courtesy of the RSNA.
"We were excited to see that the estimated cure rate we reported in 2006 has persisted after 20 years of follow-up," Henschke said.
In this analysis, the authors found that, among 1,257 I-ELCAP participants diagnosed with lung cancer, 81% had Stage I disease, and that the long-term survival rate for these patients was 87%.
By treating the cancer when it is small, patients can be effectively cured in the long term, according to Henschke. And that's why regular LDCT screening is beneficial.
"Lung cancer can be cured if you enroll in an annual screening program using a well-defined protocol and comprehensive management system," she said. "It is important to return for annual screening."
Yet even though lung cancer screening improves survival outcomes, its uptake remains low, according to an accompanying editorial written by Lecia Sequist, MD, of Harvard Medical School in Boston, and Coral Olazagasti, MD, of the University of Miami in Florida. Efforts to mitigate this must continue.
"Despite data from I-ELCAP, NLST [the National Lung Screening Trial], NELSON, and many other clinical trials suggesting lung cancer screening is beneficial and expanded guidelines from the U.S. Preventive Services Task Force that render 14.5 million Americans potentially eligible for screening, lung cancer screening implementation in the United States remains extremely suboptimal to date," they noted. "This is due to myriad systemic and individual factors compounded by stigma and nihilism about tobacco use … Concerted and long-term efforts to change the status quo for lung cancer screening are needed."
The full article is available here.




















