The percentage of lung fibrosis quantified on CT pulmonary angiograms (CTPA) by an AI model is associated with increased risk of mortality -- and boosts clinicians' ability to predict the survival of lung disease patients, researchers have found.
The information is especially useful when used in combination with radiologic severity scoring -- compared with radiologic scoring alone -- and the study findings could help clinicians better care for their patients, wrote a team led by Krit Dwivedi, PhD, of the University of Sheffield in England. The results were published February 6 in Radiology.
"There is clinical need to better quantify lung disease severity in pulmonary hypertension, particularly in idiopathic pulmonary arterial hypertension and pulmonary hypertension associated with lung disease," it noted.
The severity of lung disease is an important discriminating factor between two pulmonary hypertension types: pulmonary arterial hypertension and pulmonary hypertension associated with lung disease. But "distinguishing between these two groups is challenging in patients with radiologically scored mild or no fibrosis due to overlapping clinical characteristics, particularly in the most common form of pulmonary arterial hypertension, idiopathic pulmonary arterial hypertension," the researchers explained. "Only patients diagnosed with idiopathic pulmonary arterial hypertension are eligible for novel targeted therapies that improve survival."
Dwivedi's group conducted a study to quantify fibrosis on CTPA exams using AI and to evaluate whether the approach could be used in combination with radiologic scoring to predict patient survival. The work included a total of 521 adult patients with idiopathic pulmonary arterial hypertension or pulmonary hypertension associated with lung disease who underwent incidental CT imaging between February 2007 and January 2019; of these, 275 made up a training set and 246 a test set. The AI model quantified fibrosis on the CT exams and was also scored by radiologists.
The team found that higher, AI-quantified percentages of fibrosis translated to increased risk of patient mortality in the training cohort (hazard ratio, 1.01, with 1 as reference), a result validated in the external test cohort (C index, 0.76, with 1 as reference). Additionally, the model that combined AI-quantified fibrosis and radiologic scoring demonstrated improved performance for predicting patient mortality compared with a model that consisted of radiologic scoring alone, with a C index of 0.67 compared with 0.61 (p < 0.001).
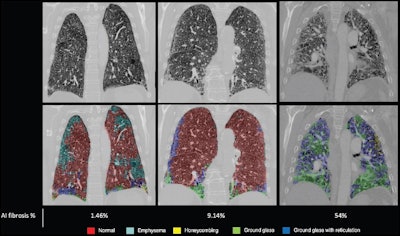 Examples of degrees of fibrosis quantified and radiologically scored. CT pulmonary angiograms (top row) were radiologically scored as having mild (left), moderate (middle), and severe (right) disease; the corresponding output and fibrosis percentage as quantified by the artificial intelligence (AI) model are shown in the bottom row. Images courtesy of the RSNA.
Examples of degrees of fibrosis quantified and radiologically scored. CT pulmonary angiograms (top row) were radiologically scored as having mild (left), moderate (middle), and severe (right) disease; the corresponding output and fibrosis percentage as quantified by the artificial intelligence (AI) model are shown in the bottom row. Images courtesy of the RSNA.
"[We found] that artificial intelligence (AI)-quantified fibrosis at CT was prognostic for survival in patients with pulmonary hypertension and lung disease," the group wrote. "This was independent of demographic characteristics … [and] hemodynamic disease severity … and was externally validated in images from 37 centers. The second key finding of our study is that the AI model was sensitive to minor parenchymal differences and, when used in combination with radiologic reporting, provided additional predictive prognostic value … [compared to] radiologic scoring alone."
The study results suggest that "further larger multi-registry prospective studies that investigate the use of such AI models in better characterizing and phenotyping patients with pulmonary hypertension and lung disease are warranted," the authors concluded.
The complete study can be found here.