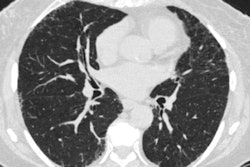
A personalized lung cancer screening model used with patients with pulmonary nodules identified on low-dose CT (LDCT) helps clinicians determine how to follow up better than rule-based protocols, researchers have found.
A group led by Zixing Wang, MD, of Peking Union Medical College in Beijing, China, found that a tailored model had a 0% rate of delayed diagnosis of lung cancer at 12-month follow-up. The results were published April 15 in Pulmonology.
Up to half of screened individuals have at least one pulmonary nodule on lung cancer screening, and determining the optimal time for follow-up testing of these nodules can be a challenge, the authors explained.
"[Finding pulmonary nodules on LDCT can be] a gateway to repeated imaging, diagnostic workup, and treatment -- including surgical resection," they noted. "Benefits of early diagnosis and treatment of cancer largely depend on criteria and frequency of follow-up examinations. However, these benefits are often offset by high overtesting rates, resource waste, complications, and mental stress. Precisely planning follow-up testing is therefore critical to improving the effectiveness of screening programs."
To address the problem, the group developed and validated a modeling schema for predicting lung cancer using data from 1,809 patients in the National Lung Screening Trial (NLST) between the ages of 55 and 74 with pulmonary nodules. Of these cases, 1,206 were used for the development of the schema and 603 for its validation. The model included predictors such as age, obesity, family history of lung cancer, smoking pack-years, and nodule information; the researchers assessed patients' cancer risk profiles at baseline and at two follow-up screening rounds, one at three months after initial screening and another at 12 months.
Overall, the team found that the personalized model showed an area under the receiver operating curve (AUROC) for predicting 12-month lung cancer onset of 0.87 at baseline screening and 0.81 at 12-month follow-up. It also reported the following:
| Performance of personalized schema for predicting lung cancer compared with NCCN and Lung-Rads | |||
|---|---|---|---|
| Measure | National Comprehensive Cancer Network (NCCN) guidelines | Lung-RADS | Personalized schema |
| At baseline screening | |||
| Rates of delayed diagnosis | 1.7% | 6.9% | 1.7% |
| Rates of overtesting | 5.6% | 5.6% | 4.9% |
| At 12-month follow-up | |||
| Rates of delayed diagnosis | 18.2% | 18.2% | 0% |
| Rates of overtesting | 8.3% | 7.3% | 2.6% |
Wang and colleagues also noted that using the tailored lung cancer prediction model translated to earlier follow-up test recommendations compared with NCCN guidelines or Lung-RADS -- especially for women, patients 65 years or older, and those individuals with part-solid or nonsolid nodules.
"The personalized schema is easy to implement and more accurate compared with rule-based protocols," the investigators concluded. "Further research is needed to examine its value in precision screening for lung cancer in diverse populations and settings."
The complete study can be found here.