To the extent that medicine is an art, sometimes there is no black and white, only shades of gray. Take cerebrovascular imaging, where choosing an exam modality such as CT angiography (CTA), MR angiography (MRA), ultrasound, or digital subtraction angiography (DSA), might hinge on a patient's age, sex, medical history -- or when all else fails, a hunch.
"When you're talking about neurovascular disease, how do you decide which to use at which time?" Dr. Jay Cinnamon asked at the 2007 International Symposium on Multidetector-Row CT in San Francisco. The answer is there, he said, if the radiologist analyzes the question by modality, by disease process, by index of concern, and through the lens of experience.
"It's all about perspective -- no hard and fast algorithmic thinking here," said Cinnamon, a neuroradiologist and director of 3D imaging at Quantum Radiology Northwest in Marietta, GA. "This is just experience. You might argue that something I suggest might go another way, and that's fine. This is the art of medicine, the art of radiology, and there's no right or wrong."
There are better and worse choices, however, and various imaging tools available to look for cerebrovascular pathology in the carotid, vertebral, and intracranial arteries. Each modality can be found somewhere along the spectrum of screening to diagnostic -- a critical question with which to approach any exam, Cinnamon said.
"When the requisition says rule out aneurysm, are you going to screen or diagnose?" he said. "If you get a patient with a family history of aneurysm and you want to screen that's one thing. But when your patient has a real subarachnoid hemorrhage, you're there to diagnose it, not screen for it."
Modality analysis
From the modality perspective, ultrasound and MRA tend toward the screening side of the equation, while DSA is diagnostic, although it could be argued that CTA is replacing DSA for some applications, and that contrast-enhanced MRA is a diagnostic tool, Cinnamon said.
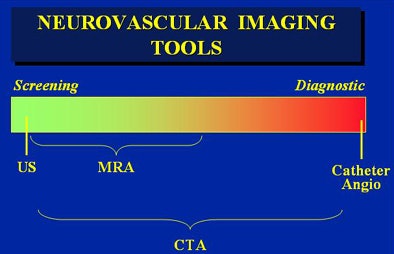 |
| Different modalities are better suited to screening or diagnosis, or both. All images courtesy of Dr. Jay Cinnamon. |
"CTA can really run the spectrum because it's minimally invasive, and it has that screening dimension to it," he said. "On the other hand, you get a lot of information so it can also move toward the diagnostic end of the spectrum."
The modality offers a handy creative framework for answering the diagnostic question, which can be further explored by asking which modality demonstrates what best, he said.
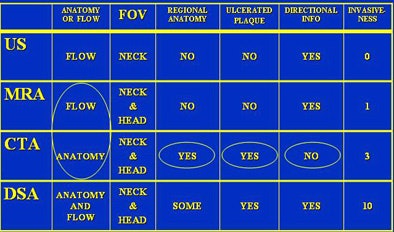 |
| Different modalities have different strengths depending on the anatomy, the patient, or suspected disease process that needs to be visualized. |
 |
In a nutshell, "MRA is looking at flow, whereas CTA is truly looking at anatomy," Cinnamon said. Thus, "MRA provides a reflection of the anatomy through the flow, whereas CTA is all about the wall of the vessel."
In fact, with time-of-flight imaging, MRA is looking at a particular kind of flow: laminar flow. MRA is challenged by more complex flow patterns such as vortex flow or turbulent flow, which can affect the modality decision, he said.
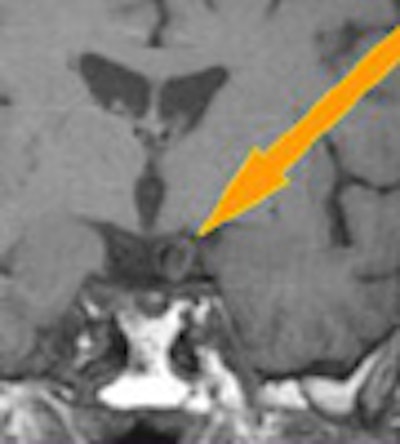
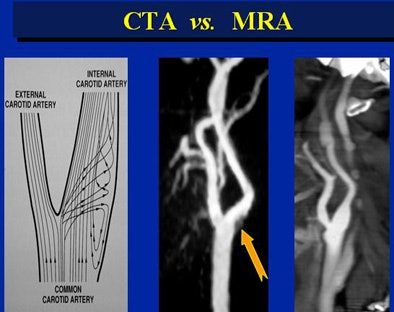 |
| Vortex flow obscured the MRA view at the bifuration of the common carotid artery (arrow). |
CTA isn't troubled by turbulence. Unfortunately, it can't tell which direction the blood is flowing. But as long as the contrast has reached the region of interest, the vessel will be opacified, Cinnamon said.
"I was burned on this once reading a patient that had a suspected subclavian steal, and I saw simultaneous opacification of the vertebral arteries. And although I was missing a little bit of subclavian artery because of streak artifact, I sort of concluded that there was no subclavian steal and I was wrong, because the blood apparently shot up one vertebral artery and came down the other vertebral artery (as shown) on the catheter angio study," he said.
MRA's flow information could have helped avoid the misread, but CTA has its own endearing qualities. "Plaque is very good with CTA, much better than some other modalities and potentially better than catheter angiography," Cinnamon said.
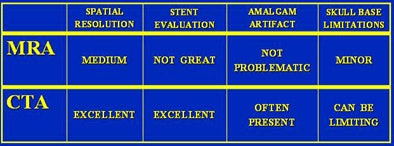
"If you look at spatial resolution, MRA is OK, CTA is better," and the same is true for stent evaluation, he said. "Stent evaluation with MRA is not great because you can get magnet susceptibilities from the stent itself that will create a flow gap on MRA."
Amalgam artifacts aren't usually a problem on MRA, and they can be a problem on CTA. But on CTA the artifacts do tend to be located away from the region of interest, minimizing potential problems. "Skull base limitations are minor in MRA, but can be limiting in CTA," he said.
CTA offers direct visualization of the vessel wall and excellent visualization of the lumen, and as a bonus, multitissue volume-rendered displays of anatomy and pathology.
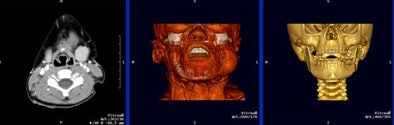 |
| CT offers some views, for example multitissue displays, that aren't available in other modalities. |
Patient analysis
The choice of modality may hinge on the patient's circumstances -- for example, in atherosclerotic disease evaluation, and requires some answers.
"Are you there to screen or diagnose disease? Are you looking in the head or neck or both?" he asked. "Is this an emergent evaluation or elective?" Are there any complicating issues such as stents?
Both requisitions say "rule out aneurysm." In a 42-year-old male with subarachnoid hemorrhage, you'll want to choose CTA, or possibly DSA, to "diagnose the aneurysm that you know is there," Cinnamon said. But in a 25-year-old woman with a family history of aneurysms, you're screening for disease, and MRA would be the better choice.
How about a 62-year-old diabetic male presenting with third cranial nerve palsy? For this patient, "the third nerve palsy might very well be due to a microinfarct of the nerve or the nucleus, and in that situation I might say do an MRA even though the suspicion (of microinfarct) is relatively low, and at the same time we're going to look at the brain stem, look at the cavernous sinus and see if there's a cavernous sinus hemangioma," Cinnamon said.
On the other hand, a 29-year-old male with third nerve palsy has an aneurysm until proved otherwise, and is sent for CTA.
What about a 58 year-old patient positive at MRI for siphon aneurysm? This patient might do best at DSA, with the argument that this modality might best demonstrate a siphon aneurysms in the bony region of the skull base, Cinnamon said.
Even race can impact the choice of modality. Say you have two 75-year-olds with a suspicious bruit on ultrasound. One is Caucasian, the other African-American.
"Caucasians tend to get atherosclerotic disease in the neck; African Americans tend to get the disease intracranially," Cinnamon said. "So in a Caucasian patient with TIA (transient ischemic attack), I might just say do an ultrasound and look at the neck. On the other hand, an African American I would do an MRA to look at the head for siphon disease, MCA disease."
Analysis by index of suspicion
The level of suspicion should also impact the choice of modality, Cinnamon said. A 50-year-old with a single episode of TIA might be sent to ultrasound, while a 50-year-old patient presenting with crescendo TIAs might be sent to CTA because of a higher index of suspicion.
Ditto for a 75-year-old man with a history of peripheral vascular disease: He is referred for CTA owing to a higher index of suspicion, Cinnamon said.
Plugging CTA at the end, Cinnamon said the modality can provide information and views, such as those found in multitissue displays, that are simply unavailable in other modalities. In a patient with an ICA stent, CTA showed the development of neointima, a predictor of restenosis, at the site on follow-up images, he said.
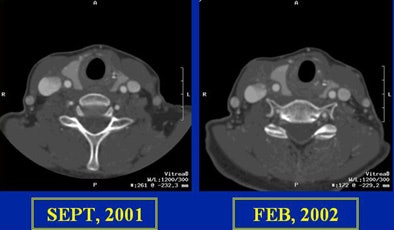 |
| In a patient with an internal carotid artery (ICA) stent, CTA showed the development of neointima, a predictor of restenosis. |
But ultrasound, CTA, MRA, and DSA all have their place in the evaluation of cerebrovascular disease. "With four great modalities ... you can rock and roll all night," Cinnamon said.
By Eric Barnes
AuntMinnie.com staff writer
July 23, 2007
Related Reading
HARM makes good on poststroke MR, exposes blood-brain barrier disruption, June 15, 2007
Small stroke centers ill-equipped for range of presentations, May 25, 2007
256-slice CT brings new possibilities in head imaging, May 28, 2007
Transient ischemic attacks can be rapidly detected, May 30, 2007
Advanced MR clarifies nexus between white matter and cerebrovascular disease, February 9, 2007
Copyright © 2007 AuntMinnie.com



















