Though results are preliminary, digital radiography tomosynthesis shows promise for diagnosing acute scaphoid wrist fractures that can lead to severe complications when missed with conventional radiography.
A pilot study by Mats Geijer, MD, and colleagues from the Center for Medical Imaging and Physiology at Skåne University Hospital in Lund, Sweden, found that tomosynthesis performed two weeks after an initial evaluation with a commercially available unit (VolumeRad option on Definium 8000, GE Healthcare, Chalfont St. Giles, U.K.) revealed three scaphoid fractures compared with one fracture uncovered when the same 35 consecutive patients were evaluated with computed radiography (CR) (FCR XG 5000, Fujifilm Medical Systems, Tokyo Japan).
The detection of two additional fractures may seem like a minor distinction, but it could make an important difference in the clinical outcomes of such patients, according to Geijer, an associate professor in the university's section for musculoskeletal radiology. Scaphoid fractures are fairly common, especially among adult men, for whom the incidence rate is 38 per 100,000. The rate for women is eight per 100,000. Scaphoid fractures account for 71% of all fractures of the carpal bones, and they usually occur when an individual extends his or her arms forward to cushion a fall.
Ninety percent of scaphoid fractures heal successfully after early diagnosis and treatment, but missed fractures may lead to nonunion or avascular necrosis of the proximal fragment. Either complication can result in scaphoid nonunion advanced collapse.
As reflected in the Appropriateness Criteria from the American College of Radiology (ACR) of Reston, VA, conventional radiography is the consensus choice for the initial evaluation of suspected scaphoid fractures. But miss rates are high -- reports in the medical literature put the miss rate at 9% to 33% -- and are variable enough to encourage caution. Standard practice calls for encasement of the wrist in a plaster cast after a negative radiograph for re-examination two weeks later.
At that point, radiologist opinion differs on the most appropriate modality to re-examine the patient for suspected occult scaphoid fracture, if symptoms and suspicions persist, Geijer and colleagues wrote. The evidence-based literature suggests MRI is most suitable because of its ability to evaluate bone marrow, according to the authors. But radiography, CT, and technetium-99m bone scans are also used. The selection of the other modalities is influenced by their cost, availability, and local medical custom, he wrote in a study was published online November 6 in the journal Skeletal Radiology.
Up to now, digital x-ray tomosynthesis has not been considered for this application. The technology has the ability to demonstrate cortical fractures and fractures of the trabecular bone with some degree of displacement, Geijer wrote. In that respect, its performance is similar to CT.
However, neither CT nor tomosynthesis can demonstrate purely trabecular bone fractures seen on T2-weighted MRI or Tc-99m bone scans. Indeed, some researchers have questioned if purely trabecular fractures or bone bruises depicted on MRI require the same treatment as cortical fractures, Geijer noted.
In the study, digital radiography was performed in the emergency department on 36 consecutive patients at the time of injury with pixel spacing of 0.1 mm. Posteroanterior (PA) and lateral views were captured. Coned-down special scaphoid views were obtained with the hand in ulnar deviation and the wrist in a slight pronation and supination, respectively, to obtain views of the proximal and distal half of the scaphoid with the x-rays perpendicular to the long axis of the bone.
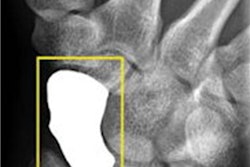
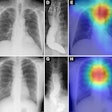
 A 20-year-old man who had initial negative wrist and scaphoid radiographs. The follow-up radiograph (a) was normal. No fractures were observed in enlargements of the wrist radiographs and two scaphoid views (b). All images reprinted with permission of Springer Publishing.
A 20-year-old man who had initial negative wrist and scaphoid radiographs. The follow-up radiograph (a) was normal. No fractures were observed in enlargements of the wrist radiographs and two scaphoid views (b). All images reprinted with permission of Springer Publishing.
Injuries were stabilized in a plaster cast for two weeks. One patient declined to participate in the trial. Follow-up imaging for the remaining 35 patients was performed at a separate site at some distance away from the ER, where CR and tomosynthesis could be performed in sequence. In actual practice, the optimal use of musculoskeletal tomosynthesis will be found by placing the equipment in the ER, Geijer noted in an e-mail to AuntMinnie.com.
The CR protocol was identical to the previous ER imaging routine. For tomosynthesis, 60 low-dose projection images were used to reconstruct tomographic sections with 1-mm nominal thickness without overlap, with a pixel spacing of 0.2 mm. The detector was stationary, while the x-ray tube was moved continuously from -17.5° to +17.5° around the standard PA position.
Two sets of studies were read by an experienced musculoskeletal radiologist and a resident radiologist, both of whom were blinded to the tomosynthesis results.
The two additional fractures identified with tomosynthesis were not statistically significant, and the decision against comparing the two modalities during the initial presentation was influenced by the inability to perform tomosynthesis in the ER. But several useful insights can still be drawn from the study, Geijer told AuntMinnie.com.
 Same patient above. With tomosynthesis (c), a nondisplaced scaphoid wrist fracture was observed in the dorsal cortex (arrows).
Same patient above. With tomosynthesis (c), a nondisplaced scaphoid wrist fracture was observed in the dorsal cortex (arrows)."Even though we did not reach significance at the two-week follow-up, we still like the increased confidence we get from the addition of tomosynthesis to conventional radiography, and the extra fractures we keep finding," Geijer said.
The trends identified in the pilot study were strong enough to conclude that tomosynthesis can detect occult fractures not visible on radiography.
"The study is noteworthy in that it has shown that radiographically occult fractures can be detected by tomosynthesis, and thus potentially reduce the number of complications after a scaphoid fracture," he wrote to AuntMinnie.com.
The experience also taught the participating radiologists that detecting fractures with tomosynthesis is somewhat different than with conventional radiography and CT. Fracture detection is mainly based on edge disruption with tomosynthesis because the structure of the medullary bone is blurred and not as distinct as in CT, Geijer noted.
The tomosynthesis sections had a "nonprecise" thickness, with a sharp resolution at the image center, and increasing "fuzziness" apparent toward the image edges.
Fracture detection was aided on the lateral borders by the ability to visualize the scaphoid bone cortex. Fractures could also be appreciated on the most dorsal and palmar sections because of good contrast between the bone and surrounding soft tissue or medullary bone, he wrote.
Image artifacts with tomosynthesis included increased noise during scaphoid imaging and the superimposition of adjacent cortical lines and carpal joint structures.
"The way a fracture is seen with tomosynthesis is thus different from both radiography and CT," he wrote.
By James Brice
AuntMinnie.com contributing writer
November 24, 2010
Related Reading
Study finds clinical niche for DR tomo in pulmonary lesions, July 28, 2010
Will new DR technologies offer alternative to CT? Part 2, March 25, 2010
Will new DR technologies offer alternative to CT? Part 1, March 24, 2010
Low-dose tomo beats chest DR for TB evaluations, March 19, 2010
Virtual dual-energy DR improves lung lesion detection, February 10, 2010
Copyright © 2010 AuntMinnie.com